Editor’s Note (12/21/21): This article is being showcased in a special collection about equity in health care that was made possible by the support of Takeda Pharmaceuticals. The article was published independently and without sponsorship.
The COVID-19 pandemic has disproportionately hurt members of minority communities in the U.S. As of April 2022, 339 Black people out of every 100,000 had died of the coronavirus, compared with 322 of every 100,000 white people. Structural racism accounts for much of this disparity. Black people are more likely to have jobs that require them to leave their homes and to commute by public transport, for example, both of which increase the chances of getting infected. They are also more likely to get grievously ill when the virus strikes. As of March 2022, the hospitalization rate for those who tested positive for SARS-CoV-2 infection was more than two times higher for Black people than for non-Hispanic white people.
One reason for this alarming ratio is that Black people have higher rates of diabetes, hypertension and asthma—ailments linked to worse outcomes after infection with the coronavirus. Decades of research show that these health conditions, usually diagnosed in adulthood, can reflect hardships experienced while in the womb. Children do not start on a level playing field at birth. Risk factors linked to maternal poverty—such as malnutrition, smoking, exposure to pollution, stress or lack of health care during pregnancy—can predispose babies to future disease. And mothers from minority communities were and are more likely to be subjected to these risks.
Today’s older Black Americans—those most endangered by COVID—are more likely than not to have been born into poverty. In 1959, 55 percent of Black people in the U.S. had incomes below the poverty level, compared with fewer than 10 percent of white people. Nowadays 20 percent of Black Americans live below the poverty line, whereas the poverty rate for white Americans remains roughly the same. Despite the reduction in income inequality between these groups, ongoing racism works through circuitous routes to worsen the odds for minority infants. For example, partly because of a history of redlining (practices through which financial and other institutions made it difficult for Black families to buy homes in predominantly white areas), even better-off Black people are more likely to live in polluted areas than are poorer white people—with a corresponding impact on fetal health. Worryingly, people disadvantaged in utero are more likely to have lower earnings and educational attainments, so that the effects of poverty and discrimination can span generations.
Researchers now have hard evidence that targeted programs can improve health and reduce inequality. Expansions of public health insurance offered to women, infants and children under Medicaid and the Children’s Health Insurance Program have had a tremendous effect, improving the health and well-being of a generation—with the largest impacts on Black children. And interventions after birth can often reverse much of the damage suffered prenatally. Along with other researchers, I have shown that nutrition programs for pregnant women, infants and children; home visits by nurses during pregnancy and after childbirth; high-quality child care; and income support can improve the outcomes for disadvantaged children. Such interventions came too late to help those born in the 1950s or earlier, but they have narrowed the health gaps between poor and rich children, as well as between white and Black children, in the subsequent decades.
Enormous disparities in health and vulnerability remain, however, and raise disturbing questions about how children born to poorer mothers during the current pandemic, with all its social and economic dislocations, will fare. Disturbingly, just before the pandemic hit, many of the most essential programs were being cut back. Between 2018 and 2020, more than a million children lost Medicaid coverage because of new work requirements and other regulations, and many became uninsured. Now that the COVID death toll has exposed stark inequalities in health status and their attendant risks, Americans must act urgently to reverse these setbacks and to strengthen public health systems and the social safety net, with special attention to the care of mothers, infants and children.
The Hunger Winter
Decades of careful observation and analysis have gone into uncovering the manifold ways in which the fetal environment affects the future health and prospects of a child, and much remains mysterious. It would be unethical to run experiments to measure the toll on a fetus of, say, malnutrition or pollution. But we can look for so-called natural experiments—the (sometimes horrific) events that cause variations in these factors in ways that mimic an actual experiment. The late epidemiologist David Barker argued in the 1980s that poor nutrition during pregnancy could “program” babies in the womb to develop future ailments such as obesity, heart disease and diabetes. Initial evidence for such ideas came from studies of the Dutch “Hunger Winter.” In October 1944 Nazi occupiers cut off food supplies to the Netherlands, and by April 1945 mass starvation had set in. Decades later military, medical and employment records showed that adult men whose mothers were exposed to the famine while pregnant with them were twice as likely to be obese as other men and were more likely to have schizophrenia, diabetes or heart disease.
Anyone born in the Netherlands during the famine is part of a cohort that can be followed over time through a variety of records. Nowadays many researchers, including me, look for natural experiments to delineate such cohorts and thereby tease out the long-term impacts of various harms experienced in utero. We also rely heavily on the most widely available measure of newborn health: birth weight. A baby may have “low” birth weight, defined as less than 2,500 grams (about 5.5 pounds), or “very low” birth weight of less than 1,500 grams (3.3 pounds). The lower the birth weight, the higher the risk of infant death. We have made enormous progress in saving premature babies, but low-birth-weight children are still at much higher risk for complications such as brain bleeds and respiratory problems that can lead to long-term disability.
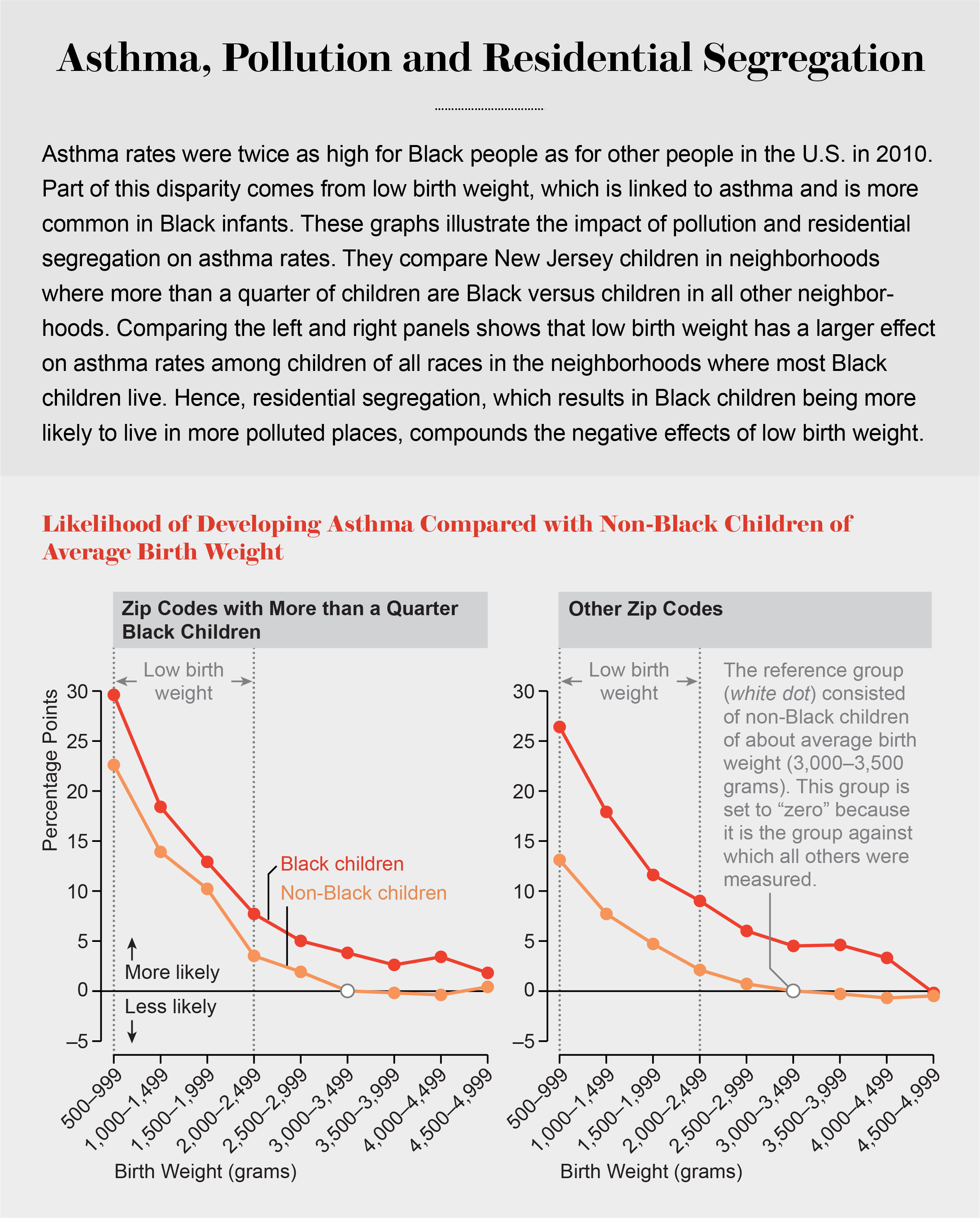
In recent years computer analysis of large-scale electronic records has made it possible to connect infant health, as measured by birth weight, to long-term outcomes not just for cohorts but also for individuals. Studies of twins or siblings, who have similar genetic and social inheritance, show that those with lower birth weight are more likely to have asthma or attention deficit hyperactivity disorder (ADHD) when they get older. Several studies also show that lower-birth-weight twins or siblings have worse scores on standardized tests. As adults, they are more likely to have lower wages, to reside in lower-income areas or to be on disability-assistance programs. In combination, cohort and sibling studies demonstrate that low birth weight is predictive of several adverse health outcomes later in life, including increased probabilities of asthma, heart disease, diabetes, obesity and some mental health conditions.
Birth weight does not capture all aspects of a child’s health: a fetus gains most of its weight in the third trimester, for example, but many studies find that shocks in the first trimester are particularly harmful. I nonetheless use the measure in my studies because it is important and commonly available, having been recorded for tens of millions of babies for decades.
Significantly, low birth weight is much more common among infants born to poor and minority mothers. In 2016 13.5 percent of Black mothers had low-birth-weight babies, compared with 7.0 percent of non-Hispanic white mothers and 7.3 percent of Hispanic mothers. Among those with college educations, 9.6 percent of Black mothers had low-birth-weight babies, compared with 3.7 percent of non-Hispanic white mothers. These inequalities in health at birth reflect large differences in exposure to several factors that affect fetal health.
The Poverty Connection
As already noted, the quality of a mother’s nutrition substantially influences the health of her babies. In 1962 geneticist James V. Neel hypothesized that a so-called thrifty gene had programmed humankind’s hunter-gatherer ancestors to hold on to every calorie they could get and that in modern times, that tendency, combined with an abundance of high-calorie foods, led to obesity and diabetes. Studies on laboratory animals indicate, however, that the link between starvation and disease is not genetic in origin but epigenetic, altering how certain genes are “expressed” as proteins. Prolonged calorie deprivation in a pregnant mouse, for example, prompts changes in gene expression in her offspring that predispose them to diabetes. What is more, the effect may be transmitted through generations.
Outright starvation is now rare in developed countries, but poorer mothers in the U.S. often lack a diet rich in fruits and vegetables, which contain essential micronutrients. Deficiencies in folate intake during pregnancy are linked to neural tube defects in children, for example.
At present, one of the leading causes of low birth weight in the U.S. is smoking during pregnancy. In the 1950s pregnant women were told that smoking was safe for their babies. Roughly half of all new mothers in 1960 reported smoking while pregnant. Today, thanks to public education campaigns, indoor-smoking bans and higher cigarette taxes, only about 6 percent of pregnant women say that they smoke. And 54 percent of women who smoked in the three months before they got pregnant quit for at least the duration of their pregnancy.
Possibly because going to college places women in a milieu where smoking is strongly discouraged, mothers with higher education levels are less likely to smoke. Among mothers with less than a high school education, 11.2 percent smoke, compared with fewer than 1 percent of mothers with a bachelor’s degree.
Among the many harmful chemicals in cigarette smoke is carbon monoxide (CO), which restricts the amount of oxygen carried by the blood to the fetus. In addition, nicotine affects the development of blood vessels in the uterus and disrupts developing neurotransmitter systems, leading to poorer psychological outcomes. Maternal cigarette smoking during pregnancy has also been associated with epigenetic changes in the fetus, although how these alterations affect an individual in later years remains mysterious. Vaping, which has surged since 2010, delivers high doses of nicotine, and surveys show that it has been tried by almost 40 percent of high school seniors. This rise in popularity is extremely alarming because it could have long-term implications for fetal and infant health.
Yet another significant source of harm for fetuses is pollution. Pregnant women may be exposed to thousands of toxic chemicals in the air, water, soil and sundry products at home and at work. Complicating matters, each pollutant acts in a different way. Particulates in the atmosphere are thought to cause inflammation throughout the body, which has been linked to preterm labor and, consequently, to low birth weight. Lead, ingested through water or air, crosses the placenta to accumulate in the fetus and harm brain development. In 2005 Jessica Wolpaw Reyes of Amherst College showed that the phaseout of leaded gasoline in the U.S. led to a decrease of up to 4 percent in infant mortality and low birth weight.
A fetus may also receive less oxygen if its mother inhales CO from vehicle exhaust. In a 2009 study of mothers who lived near pollution monitors, my co-workers and I found that high levels of ambient CO were correlated with reduced birth weight. Worryingly, the effects of CO from air pollution are five times greater for smokers than for nonsmokers.
Reducing pollution can have immediate benefits for pregnant women and newborns. In a 2011 study of babies born in New Jersey and Pennsylvania, Reed Walker of the University of California, Berkeley, and I focused on mothers who lived near E-ZPass electronic toll plazas before and after they began operating. We compared them with mothers who lived a little farther from the toll plazas but along the same busy roads. Both groups of mothers were exposed to traffic, but before E-ZPass, the mothers near the toll plazas were exposed to more pollution because cars idled while waiting to pay the tolls. E-ZPass greatly reduced pollution right around the toll plazas by allowing cars to drive straight through. Startlingly, the introduction of E-ZPass reduced the incidence of low birth weight by more than 10 percent in the neighborhoods nearest the toll plazas.
In another study, my collaborators and I examined birth records for 11 million newborns in five states. We found that a shocking 45 percent of mothers lived within about a mile of a site that emitted toxic chemicals such as heavy metals or organic carcinogens—a number that rose to 61 percent among Black mothers. Focusing on babies born to mothers who lived within a mile of a plant, we compared birth weights when the facility was operating with birth weights when it was closed. For additional context, we also compared babies born within a mile of a plant with babies born in a one-to-two-mile band around the plants. Both groups of mothers were likely to be similarly affected by the economics of factory openings and closings, but mothers who lived closer were more likely to have been exposed to pollution during pregnancy. We found that an operating plant increased the probability of low birth weight by 3 percent among babies whose mothers lived less than a mile from the plant.
The racial divide in pollution exposure is profound, in part because of continuing segregation in housing that makes it difficult for Black families to move out of historically Black neighborhoods. Disadvantaged communities may also lack the political power to fend off harmful development, such as a chemical plant, in their vicinity. In the E-ZPass study, roughly half of the mothers who lived next to toll plazas were Hispanic or Black, compared with only about a tenth of mothers who lived more than six miles away from a toll plaza. And in a paper published in 2020, John Voorheis of the U.S. Census Bureau, Walker and I showed that across the entire U.S., neighborhoods with higher numbers of Black residents have systematically worse air quality than other neighborhoods. Black people are also twice as likely as others to live near a Superfund hazardous waste site. For these reasons, pollution-control measures such as the Clean Air Act have greatly benefited Black people.
Fight or Flight
Stress disproportionately impacts the poor—who have chronic worries about paying bills, for example—and also harms fetuses. A stressful situation triggers the release of hormones that orchestrate a range of physical changes associated with the fight-or-flight response. Some of these hormones, including cortisol, have been linked to preterm labor, which in turn leads to low birth weight. High circulating levels of cortisol in the mother during pregnancy may damage the fetus’s cortisol-regulation system, making it more vulnerable to stress. And stress can trigger behavioral responses in a mother such as increased smoking or drinking, which are also harmful to the fetus.
One revealing study indicates that fetal exposure to maternal stress can have greater negative long-term effects on mental health than stress directly experienced by a child. Petra Persson and Maya Rossin-Slater, both at Stanford University, looked at the impact of the death of a close relative. Death can bring many unwelcome changes to a family, such as reduced income, which may also influence child development. To account for such complications, the researchers used administrative data from Sweden to compare children whose mothers were affected by a death during the prenatal period with those whose mothers were affected by a death during the child’s early years. They found that children affected by a death prenatally were 23 percent more likely to use medication for ADHD at ages nine to 11 and 9 percent more likely to use antidepressants in adulthood than were children whose families experienced a death a few years after their birth.
Another pathbreaking study measured levels of cortisol, an indicator of stress, during pregnancy. By age seven, children whose mothers had higher cortisol levels during pregnancy had received up to one year less schooling than their own siblings, indicating that they had been delayed in starting school. Moreover, for any given level of cortisol in the mother’s blood, the negative effects were more pronounced for children born to less educated mothers. This finding suggests that although being stressed during pregnancy is damaging to the fetus, mothers with more education are better able to buffer the effects on their children—an important finding in view of the severe stress imposed by COVID on families today.
It is no surprise that disease can also harm a fetus. Douglas V. Almond of Columbia University looked at people born in the U.S. at the peak of the influenza epidemic of 1918 and found that they were 1.5 times more likely to be poor as adults than were those born just before them. In work I conducted with Almond and Mariesa Herrmann of Mathematica looking at mothers born between 1960 and 1990 in the U.S., we found that women who were born in areas where an infectious disease was raging were more likely to have diabetes when they gave birth to their own children decades later—and the effects were twice as large for Black people.
More recently, Hannes Schwandt of Northwestern University examined Danish data and found that maternal infection with ordinary seasonal influenza in the third trimester doubles the rate of premature birth and low birth weight, and infection in the second trimester leads to a 9 percent reduction in earnings and a 35 percent increase in welfare dependence once the child reaches adulthood.
Preventing Harm
Health at birth and beyond can nonetheless be improved through thoughtful interventions targeting pregnant women, babies and children and through reductions in pollution. The food safety net in the U.S. has already had tremendous success in preventing low birth weight in the babies of disadvantaged women. The rollout of the food stamp program (now called the Supplemental Nutrition Assistance Program, or SNAP) across the U.S. in the mid-1970s reduced the incidence of low birth weight by between 5 and 11 percent. In addition, children who benefited from the rollout grew up to be less likely to have metabolic syndrome—a cluster of conditions that include obesity and diabetes. Notably, women who had benefited as fetuses or young children were more likely to be economically self-sufficient.
The 1970s also saw the introduction of the Special Supplemental Nutrition Program for Women, Infants and Children, popularly known as WIC. Approximately half of eligible pregnant women in the U.S. receive nutritious food from WIC, along with nutrition counseling and improved access to medical care. Dozens of studies have shown that when women participate in WIC during pregnancy, their babies are less likely to have low birth weight. In work looking at mothers in South Carolina, Anna Chorniy of Northwestern, Lyudmyla Ardan (Sonchak) of Susquehanna University and I were able to show that children whose mothers received WIC during pregnancy were also less likely to have ADHD and other mental health conditions that are commonly diagnosed in early childhood.

In the late 1980s and early 1990s, state and federal governments worked together to greatly expand public health insurance for pregnant women under the Medicaid program. In work with Jonathan Gruber of the Massachusetts Institute of Technology, I showed that public health insurance lowered infant mortality and improved birth weight. Today the children whose mothers became eligible for health insurance coverage of their pregnancies in that period have higher levels of college attendance, employment and earnings than the children of mothers who did not. They also have lower rates of chronic conditions and are less likely to have been hospitalized. The estimated effects are strongest for Black people, who, having lower average incomes, benefited the most from the expansions. The fact that these babies are more likely to eventually get a college education also increases the life chances of their children. In the U.S., an additional year of college education for the mother reduces the incidence of low birth weight in her children by 10 percent.
Even so, too many children are still born with low birth weight, especially if their mothers are Black. Significantly, targeted interventions after birth can improve their outcomes. Programs such as the Nurse-Family Partnership provide home visits by nurses to low-income women who are pregnant for the first time, many of whom are young and unmarried. The nurse visits every month during the pregnancy and for the first two years of the child’s life to provide guidance about healthy behavior. The assistance reduces child abuse and adolescent crime and enhances children’s academic achievement.
Providing cash payments to poor families with young children also improves both maternal health and child outcomes, suggesting that COVID relief payments will have important protective effects. In the U.S., the largest preexisting program of this type is the Earned Income Tax Credit (EITC). Studies of beneficiaries of the EITC show that children in families that received increased amounts had higher test scores in school. With financial stress being somewhat relieved, the mental health of mothers in these families also improved. In addition, quality early-childhood education programs augment future health, education and earnings and reduce crime. Head Start, the federally funded preschool program that was rolled out beginning in the 1960s, has also had substantial positive effects on health and education outcomes, especially in places with less access to alternative child care centers.
A 2018 study, especially noteworthy in light of the tragic lead poisoning in Flint, Mich., shows that even some of the negative effects of lead can be reversed. In Charlotte, N.C., lead-poisoned children who received lead remediation, nutritional and medical assessments, WIC and special training for their caregivers saw reductions in problem behaviors and advanced school performance.
Looking Ahead
Investments in pregnant women and infants have been paying off, their success reflected in dramatically falling infant mortality rates in the U.S.—despite rising inequality in income and wealth. Alarmingly, however, many successful programs, such as the Clean Air Act, SNAP and Medicaid, are under attack. The Coronavirus Aid, Relief and Economic Security (CARES) Act passed in March 2020 provided some relief, at least with respect to Medicaid. CARES temporarily suspended disenrollment from the program, giving additional flexibility to state Medicaid programs in terms of time lines and eligibility procedures. Still, states may be hard-pressed to enroll the many who will become newly eligible for Medicaid because of job loss. Moreover, states that have not expanded the Medicaid program to cover otherwise ineligible low-income adults, as allowed by the Affordable Care Act, may see many more uninsured.
A National Academies of Sciences, Engineering and Medicine report published in 2019 laid out a road map for reducing child poverty by half within 10 years. One of the most stunning findings of the report is that it is feasible to meet that target by expanding programs that already exist. Following these directions would have a profound impact on health and health disparities. Targeted approaches, such as more thorough investigation of maternal deaths occurring up to one year after a birth, are also necessary. Even simple preventive measures such as giving pregnant women flu shots can have a tremendously positive effect on infant health and child development. Diagnosis and treatment of conditions such as preeclampsia (high blood pressure associated with pregnancy) are key to both protecting babies and lowering maternal mortality rates. It is important to help pregnant women quit smoking and to develop new approaches relevant to a new generation addicted to vaping. Also needed are stronger protections for women at risk of domestic violence, which leads directly to chronic stress, premature deliveries and low birth weight.
One salient open question is what effect the pandemic will have on the generation of children affected by it in utero and in early life. COVID itself may have negative effects on the developing fetus. The latest data suggest that although the overall risk is low, pregnant women are at increased risk of becoming critically ill (as they are with influenza or SARS). Affected babies, however, do not seem to be at risk of obvious birth defects (as they are with the Zika virus). Still, given the fact that COVID affects many body systems, it may prove to have subtler negative effects on the developing fetus. The pandemic is also an extremely stressful event compounded by the sharpest economic downturn since the Great Depression. The years 2020 and 2021 saw marked increases in domestic violence, alcohol consumption and drug overdoses, all of which are known to be harmful to the developing fetus. In consequence, the generation being born now is likely to be at increased risk going forward and will require intensive social investments to overcome its poorer start in life.
In a July 2020 sermon on the late civil rights leader John Robert Lewis, Reverend James Lawson recounted the significant gains for Americans of all colors that had resulted from that movement. He went on to ask that America’s political leaders “work unfalteringly on behalf of every boy and every girl, so that every baby born on these shores will have access to the tree of life ... let all the people of the U.S.A. determine that we will not be quiet as long as any child dies in the first year of life in the United States. We will not be quiet as long as the largest poverty group in our nation are women and children.” As we rebuild our shattered safety nets and public health systems in the aftermath of COVID, we need to seize the moment and use the knowledge we have gained about how to protect mothers and babies—to give every child the opportunity to flourish.