It takes Lawrence Tabak about 15 minutes to rattle off all the potential COVID-19 treatments being tested in the clinical trial programme he oversees: a lengthy, tongue-twisting list that includes drugs to disarm the virus, to soothe inflammation and to stop blood clots. Over the past two years, the ACTIV programme, run by the US National Institutes of Health (NIH), has included more than 30 studies—13 of them ongoing—of therapeutic agents chosen from a list of 800 candidates. Several of the studies are due to report results in the first half of the year.
And that’s just in his programme; hundreds more are in progress around the world. Whether those results are positive or negative, Tabak says, 2022 is poised to provide some much-needed clarity on how best to treat COVID-19. “The next three to four months are, we hope, going to be very exciting,” says Tabak, acting director of the NIH in Bethesda, Maryland. “Even when a trial does not show efficacy, that’s still incredibly important information. It tells you what not to use.”
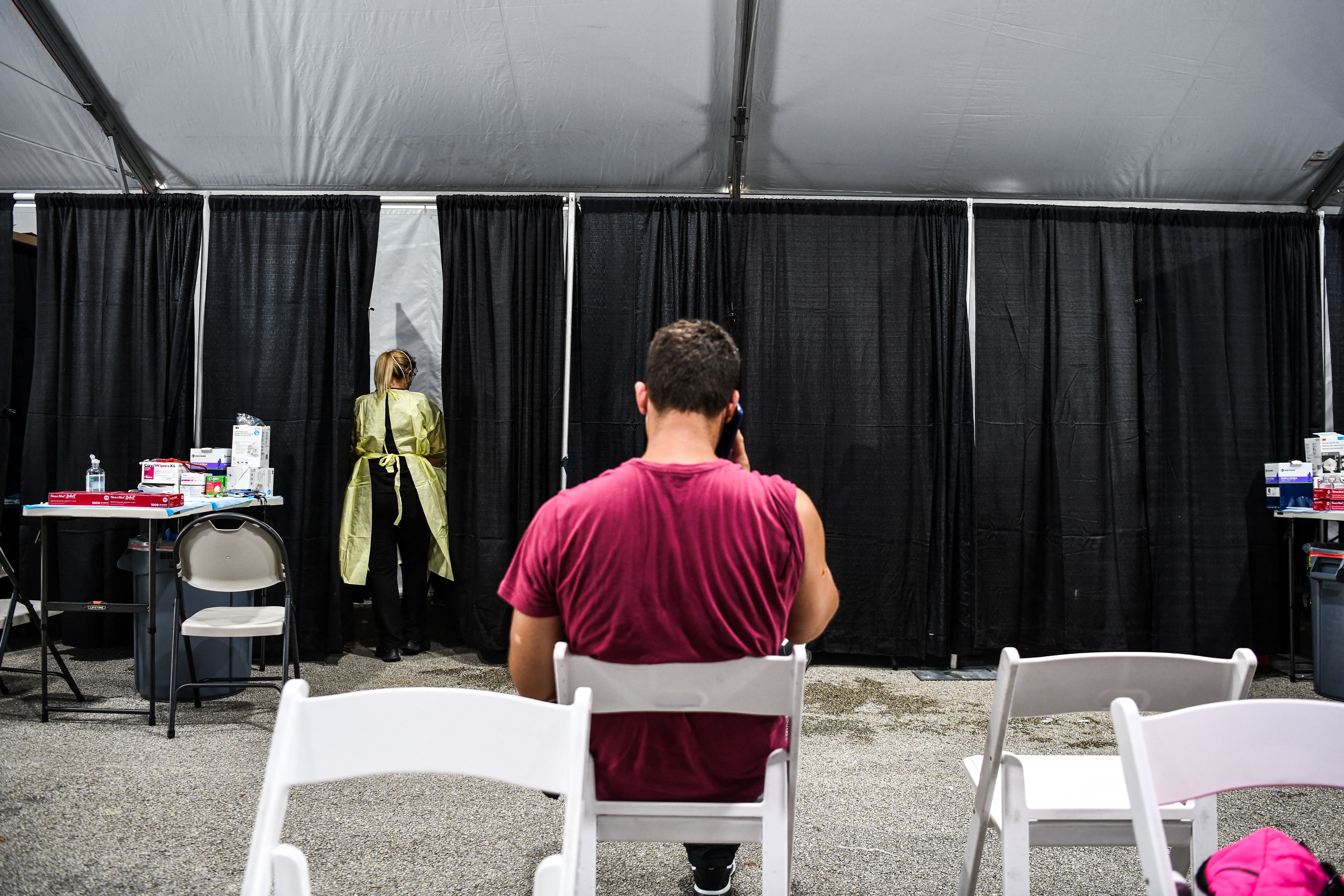
Nearly two years into the pandemic, that information is still badly needed: with more than one million new infections and thousands of deaths around the world each day, COVID-19 continues to strain health-care systems and exact a terrible human toll. Researchers have developed a handful of options—including two oral antiviral drugs, Paxlovid and molnupiravir, authorized in some countries in the past couple of months—that help in certain situations. But gaps remain, and researchers think that this year will bring new drugs and new uses for older drugs, including better treatments for mild COVID-19.
And although vaccines remain the most important way to rein in the pandemic, there is still a desperate need for better therapies to treat people who cannot—or choose not to—access the vaccines, whose immune systems cannot respond fully to vaccination, or who experience breakthrough infections. “The main tool in combating the pandemic is prevention, and the main tool in prevention is vaccination,” says Taher Entezari-Maleki, who studies clinical pharmacy at Tabriz University of Medical Sciences in Iran. “But new medications can fill in when vaccines do not work—for example against new variants.”
Over time, researchers have ramped up clinical-trial infrastructure, and repeated surges of the coronavirus SARS-CoV-2 have ensured a ready pool of potential study participants. The result has been an accelerated drug pipeline, says Tabak (see ‘Bursting pipeline’). “It has been two years, which feels like a long time for everybody,” says Paul Verdin, head of consulting and analytics at the London-based pharmaceutical analytics firm Evaluate. “But in the grand scheme of drug development, that’s not very long.”
Trickle becomes flood
Early in the pandemic, much research focused on finding ways to treat people who were seriously ill with COVID-19, to save lives and ease pressures on hospitals. In mid-2020, scientists found that a steroid called dexamethasone tamps down supercharged immune responses that can contribute to late stages of severe disease, and reduces deaths in people in this group. Such steroids remain the most effective treatments for reducing COVID-19 deaths.
Other drugs target the virus more directly but must be administered by medical professionals, limiting their use. The antiviral drug remdesivir (Veklury), made by Gilead Sciences in Foster City, California, is given as an infusion, and so was reserved, until recently, only for people hospitalized with COVID-19. (On 21 January, the US Food and Drug Administration (FDA) authorized remdesivir for outpatient treatment of people at high risk of COVID-19 complications.)
Several firms have developed monoclonal antibodies—mass-produced versions of the neutralizing antibodies that the immune system pumps out to bind to and disable SARS-CoV-2. These therapies offered another early route to treatment, and more than 200 monoclonal antibodies are now under development or authorized. But they are expensive compared with other treatments, are in short supply, and often have to be infused. One recent exception is a long-lasting combination of two monoclonal antibodies, called Evusheld. This drug, made by AstraZeneca in Cambridge, UK, can be injected into muscle, and was authorized by the FDA last December for prevention of COVID-19 in people at high risk of exposure to SARS-CoV-2.
With time, the focus began to shift to drugs that could be used outside a hospital setting to treat mild illness, in the hope of preventing progression to more severe disease. In late 2021, two antiviral treatments—Lagevrio (molnupiravir), developed by Merck, based in Kenilworth, New Jersey, and Ridgeback Biotherapeutics in Miami, Florida; and Paxlovid (a combination of two drugs, nirmatrelvir and ritonavir), developed by Pfizer, based in New York City—became available as pills that could be taken at home.
Neither drug is a panacea, notes José Carlos Menéndez Ramos, who studies pharmacy at the Complutense University of Madrid. A laboratory study has suggested that molnupiravir might be able to cause mutations in human DNA, leading regulators to advise against its use during pregnancy. Some countries, including France and India, have chosen not to authorize it. And Paxlovid’s use could be limited because it might interact with a wide range of commonly used medications.
Luckily, the two could soon have company. Many antivirals in trials target one of two key viral proteins, with the aim of stopping the virus from replicating. Like molnupiravir, some of these target a protein called RNA-dependent RNA polymerase. About 40 candidates are under development, says Chengyuan Liang, who studies pharmacy at Shaanxi University of Science and Technology in Xi’an, China. Another roughly 180 molecules act like Paxlovid and block the SARS-CoV-2 main protease protein, which is responsible for clipping viral proteins into their final, functional forms. Of these protease inhibitors, the one that has progressed furthest is S-217622, made by Shionogi in Osaka, Japan, which is in late-stage clinical trials.
.jpg)
Other antiviral medications with a fresh set of targets are working their way along the pipeline. Some of them have been selected to block the human proteins that SARS-CoV-2 uses to infiltrate cells, rather than viral proteins. For example, a cancer drug called plitidepsin targets a human protein called eEF1A, which is involved in making proteins and is important for the replication of several viral pathogens. Plitidepsin has been shown to reduce SARS-CoV-2 replication in mice, and is now in phase III clinical trials.
Targeting human proteins such as eEF1A could make it more difficult for the virus to mutate to evade the drug than when viral proteins are the target, says Ramos. “On the flip side, targeting a host protein can lead to toxicity,” he adds. In the case of plitidepsin, Ramos is hopeful that the dose required to restrict SARS-CoV-2 replication is low enough, and treatment duration short enough, for the drug to be a safe antiviral.
Researchers hope to target a smattering of other viral and human proteins important for SARS-CoV-2 replication. For example, the drug camostat, made by Ono Pharmaceutical in Osaka, inhibits a human protease, called TMPRSS2, that SARS-CoV-2 and several other coronaviruses use to enter human cells. Camostat is already used in Japan to treat non-viral conditions such as pancreatitis.
New combinations
Some familiar COVID-19 antivirals could find fresh uses, either in a formulation that makes them easy to administer, or in different patient groups. Antivirals such as remdesivir seem to work best when given earlier in the course of infection, before severe disease sets in; researchers are working on oral formulations to see whether this definitely is the case.
Conversely, researchers also want to know whether the new oral antivirals could improve outcomes for people with severe COVID-19. Clinical trials of molnupiravir in people who have been hospitalized have suggested that these drugs would not work against moderate or severe illness, when the immune system is contributing to the damage. But epidemiologist and infectious-disease specialist Peter Horby at the University of Oxford, UK, says that the studies of people in hospital might have been too small for researchers to draw a firm conclusion. It’s a common problem during the pandemic, he says: many investigators launched quick, small trials, enrolling too few participants to yield clear answers. Some treatments were abandoned prematurely. “The studies weren’t big enough, and stuff was being ditched way too early in our opinion,” he says.
Horby is one of the lead investigators on the UK RECOVERY trial—a large, multitherapy trial in people hospitalized with COVID-19. RECOVERY will test molnupiravir and eventually Paxlovid, he says. Treating sicker people could be the best way to make the most of these scarce drugs. Most infected people won’t develop severe disease and there is no definitive way to tell who will; giving the drug to people with mild disease might not yield as much benefit as treating those who are severely ill. While supplies of the drugs are low, he says, “you’ve got to target your use of a limited and expensive resource”.
The RECOVERY trial will also begin to unpick whether these antivirals work synergistically when given together. Some participants in the trial will receive one of the drugs; others might receive a combination of the two, or one of the antivirals together with a monoclonal antibody. Researchers hope that combining antivirals can boost their effectiveness and reduce the chances that the virus will develop resistance to the drugs. “We don’t have many antiviral options,” says Horby. “If we lost any, it would be a disaster.”
Researchers are exploring other options for those hospitalized with COVID-19. Treatments at this late stage often focus on the immune system, which, whipped into a frenzy by the viral infection, can begin to harm the body’s own tissues. Anti-inflammatory drugs are top of the list. RECOVERY is now looking at higher doses of steroids such as dexamethasone, and several trials are studying whether diabetes drugs called SGLT2 inhibitors—also thought to have anti-inflammatory properties—help people with moderate to severe COVID-19.

Reuse and repurpose
Globally, some of the most important trials are those that study widely available drugs developed to treat other diseases. For Philippe Guérin, director of the Infectious Diseases Data Observatory at the University of Oxford, it has been frustrating to see that many large clinical trials are focused on therapies that, in a lot of countries, will be too expensive to buy or too difficult to administer. “There is a clear disconnect between the needs of lower- to middle-income countries and the level of research,” he says. “Most of the large funding was focused on the needs of high-income countries.”
This was reflected in the early attention given to people with severe COVID-19, who were coming to hospitals and being treated in intensive care units (ICUs). “In low-income countries, you don’t have ICU capacity,” says Guérin. “What you want to do is try to prevent the non-severe patients from becoming severe, and that was not clearly the priority of the funders.”
Much of the early research on treating mild COVID-19 focused on monoclonal antibodies, notes public-health specialist Borna Nyaoke, clinical operations representative for East Africa at the Drugs for Neglected Diseases initiative, a non-profit organization in Nairobi. But these drugs pose a challenge in lower- and middle-income countries, she says, because of their cost, and because they need to be stored at low temperatures and administered by trained medical personnel. And the newer, oral antivirals promise to be less expensive, but are still in short supply.
For more practical solutions, Nyaoke looks to the ANTICOV trial, which is enrolling participants in 19 sites across 13 countries in sub-Saharan Africa. The trial is looking at a range of repurposed treatments, including the anti-parasitic drug ivermectin; an inhaled steroid called budesonide; and the antidepressant fluoxetine. (Other trials, including one run by ACTIV, are testing a similar antidepressant, called fluvoxamine, which has shown promise in some early clinical trials.)
Some of these treatments have already been tested—and sometimes failed—in smaller clinical trials. Ivermectin, in particular, has become a popular but controversial COVID-19 treatment in many countries, despite clinical trials indicating that the drug does not work as an antiviral in early stages of infection. Both ACTIV and ANTICOV are testing the treatment anew. ACTIV is running a trial in people with mild to moderate COVID-19, and results are due in the next few months. “No matter what we find, that will be of interest to many people,” says Tabak. The ANTICOV trial will test ivermectin for its potential anti-inflammatory properties in people seriously ill with COVID-19, and will combine it with an antimalarial drug. Preclinical data have been promising, says Nyaoke. “Combining drugs with different mechanisms of action increases a treatment’s chances of success,” she says.
Drug developers still face challenges when it comes to finding COVID-19 therapies. For instance, there is a shortage of non-human primates to use for research, and the costs of animals have skyrocketed, says Liang.
And although clinical-trial planners are not short of participants, running a trial in a pandemic is complicated: emerging viral variants can change the spectrum of symptoms, the severity of disease and the population that’s most affected. In some cases, variants have rendered COVID-19 therapies—particularly some of the monoclonal antibodies—obsolete. By contrast, broader-acting drugs such as remdesivir, which was developed in 2015 and tested against severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS) in animal models, and against Ebola in humans, could be useful tools in future pandemics. In the middle of this chaos, it’s hard to know which of the many therapies in current trials will be successful, says Verdin. “The whole thing is such a big churning bubble; the goal posts are constantly moving,” he says. “It’s very difficult to pick a winner.”
This article is reproduced with permission and was first published on March 1 2022.


