The heat of the sun, a blazing basketball in the West African sky, was softened by a spring breeze one afternoon a few years ago. Every so often the wind whisked a mango off a tree branch and dropped it with a thud on the corrugated iron roof that covered the health center in Bissau, the biggest city in the tiny country of Guinea-Bissau, where the rust-colored ground hadn’t felt a raindrop in six months. Inside the building, the air was still and dry, and a line of women and toddlers were sticky with sweat.
An 18-month-old named Maria with thick, dark braids studied me nervously as she perched on her mother’s lap. (The child’s name has been changed to protect her privacy.) Next to them, Carlito Balé, a soft-spoken doctor in a short-sleeved, white button-down shirt, talked with Maria’s mother in Portuguese creole, a percussive fusion of Portuguese and African dialects. Balé was telling the mother that Maria was eligible to participate in a clinical trial to test whether an extra dose of measles vaccine prevented not just the measles but many childhood infections that cause serious illness and death.
In the U.S., where life-threatening infections are rare, such a trial might not garner many volunteers. But in Guinea-Bissau, where lives have been scarred by decades of scant resources and poor medical care, families lined up for it. The nation is one of the world’s poorest, and the CIA ranks infant mortality there as the fourth highest among 225 countries. Mothers often wait months to name their babies because one out of every 12 will die before his or her first birthday.
The researchers leading the trial—anthropologist Peter Aaby and physician Christine Benn, whom I had traveled to Guinea-Bissau to meet—have amassed evidence that a few specific vaccines can thwart a multitude of threatening plagues. Over decades they have published hundreds of studies suggesting that live, attenuated vaccines, which are made from weakened but living viruses or bacteria, can stave off not just their target infections but other diseases, such as respiratory infections (including pneumonia), blood infections (including sepsis) and diarrheal infections. In a 2016 review published in the journal BMJ, a research team commissioned by the World Health Organization analyzed 68 papers on the topic, many of which came from Aaby and Benn’s research. It concluded that the measles and tuberculosis vaccines “reduce overall mortality by more than would be expected through their effects on the diseases they prevent.” Some of the research the team evaluated linked the measles vaccine with a whopping 50 percent lower risk of death from any cause.
This notion that live vaccines have what are called “off-target” effects—and powerful ones—has implications that stretch far beyond Africa. In 2017 in the U.S., for instance, researchers at the Centers for Disease Control and Prevention reported that children were half as likely to be hospitalized for nonvaccine-targeted infections between the ages of 16 and 24 months if the last immunization they had received was a live vaccine rather than an inactivated one. Recent research in immunology suggests that live vaccines can have such wide-ranging effects because they stimulate a part of the immune system that fights a broad-based war against all outside invaders, giving the system a head start on defense. “Although we still need to know much more about the details, I now have no doubt that vaccines do have some off-target effects because of the support from many different types of evidence,” says Frank Shann, a pediatrician at Royal Children’s Hospital Melbourne in Australia.
Yet other scientists are far less certain. Aaby and Benn’s work is, in fact, quite controversial. For one thing, most of the studies from the two Danish researchers do not prove cause-to-effect connections. “Purported effects” is how Paul Fine, an infectious disease epidemiologist at the London School of Hygiene & Tropical Medicine, describes them. Kids who get live vaccines might survive longer for reasons that have nothing to do with immunizations: the children in those groups might have been healthier to begin with. To address these concerns, Aaby and Benn have been running intervention trials, such as the one Maria was being recruited for. In it, children will be matched for age and basic health, but some will have only the standard single measles shot at nine months, whereas others will get an additional dose as toddlers.
The two investigators also counter that political and pragmatic concerns drive resistance to their ideas far more than do valid scientific critiques. Aaby says that his and Benn’s research is inconvenient for public policy because it indicates that live vaccines should be given last in any vaccine series, which upends current immunization schedules and could inadvertently trigger parental worries about safety. Public health scientists “don’t want to hear it, and I can understand why they don’t want to hear it,” Aaby says. And as a result, he claims, many orthodox vaccine researchers “have clearly made me persona non grata.” The 77-year-old, who is bespectacled and has a salt-and-pepper goatee, fits the part of the eccentric, obstinate and misunderstood scientist so well that he has literally become one in a novel: he inspired a character in a best-selling 2013 Danish mystery book, The Arc of the Swallow, who gets murdered in the first chapter.
In real life, Aaby and Benn’s ideas may be reaching a tipping point. The WHO wrote in a 2014 report that nonspecific vaccine effects seem “plausible and common” and worthy of more attention. Therefore, in April 2017 the agency announced it would oversee the design of two multiyear clinical trials to further test the hypothesis, although those trials have not yet begun.
The two researchers, whose professional relationship has evolved into a long-term romantic one, are pushing forward with more of their own trials, too. One of them is the study Maria’s mother was considering. As I watched in the health center, she decided to enroll her daughter, so Balé picked up a large envelope containing dozens of smaller sealed envelopes and held it open toward her, telling her to pick one—a step that ensured that her daughter would be randomly allocated to either the treatment or control group. Opening her chosen envelope, Balé announced that Maria would get the extra vaccine, and her mother flashed a hopeful smile. She carried her daughter into the next room, where a nurse in a long, white-and-orange tie-dyed dress, black glasses and a kind smile waited with a needle.
The Measles Clue
In 1979, soon after launching a health surveillance project in Bissau, a young Aaby watched measles kill one out of every four babies in the area. That was the year he saw his first dead body, and he saw a lot more than one.
Back then, childhood vaccines were rare in Africa. The WHO estimates that in 1980, only 6 percent of African children received the first dose of live measles vaccine, and 8 percent got the first inactivated DTP vaccine, which protects against diphtheria, tetanus and pertussis. It’s not as if the vaccine was new; the combination DTP vaccine was licensed in 1949, yet 31 years later fewer than one in 12 African children ever received a dose. Indeed, only a handful of childhood vaccines were even available then in Africa. In addition to the DTP and measles vaccines, there was a live tuberculosis vaccine called bacillus Calmette-Guérin (BCG) and a live polio vaccine. In 1980 in the U.S., on the other hand, 86 percent of kids received the live measles vaccine, 98 percent were inoculated with the inactivated DTP vaccine, and 95 percent had gotten live polio vaccines. African children today receive a lot more vaccines than they used to, but they still woefully lag behind the U.S.

In 1978, a year before the historic measles outbreak began, Aaby had been sent to Guinea-Bissau by a Swedish organization to investigate malnutrition. When the epidemic swept into the city, he pulled strings to import measles vaccines and began to inoculate the local children, all the while keeping track of infection and death rates. The move was a bold one: at that time, public health authorities thought that measles vaccine campaigns in Africa were essentially a waste of money and effort. In a 1981 paper published in the Lancet, researchers analyzed survival data after undertaking a measles vaccine campaign in Zaire and concluded that in the future, “it may be useful to think twice before allocating already scarce resources to such a programme.” Measles took the lives of the weakest children, they argued; even if the vaccine prevented the infection, the spared children would die from something else soon enough.
Aaby’s experience didn’t support this argument. The before-and-after numbers he saw were staggering: In 1979, the first year of the outbreak, 13 percent of local children between the ages of six months and three years died; in 1980, when the measles vaccine was available, only 5 percent did. Surprisingly, deaths from causes other than measles dropped by one fifth between 1979 and 1980, too. The trend continued. Even after measles disappeared, immunized children remained more likely than their unvaccinated peers to survive other infections. “It was one of those moments where you can suddenly see something you would never have believed was possible,” he recalls. Aaby and his colleagues wrote a letter to the Lancet refuting the theory that measles inoculation campaigns in Africa were useless—his first-ever publication in a medical journal. After that, he says of the measles vaccine, “I became obsessed.”
Aaby has now published more than 100 studies on this one vaccine. His surveillance program, the Bandim Health Project, a collaboration between Guinea-Bissau’s Ministry of Health and the University of Southern Denmark, is one reason why. For more than 40 years the project has been registering all pregnancies, births and deaths in Bissau’s urban district of Bandim, as well as in five nearby rural regions. Aaby’s team there has monitored the health of more than 500,000 people living in these areas and has collected data on hospitalizations, vaccinations and health-related choices, such as whether people sleep with mosquito nets. One day during my visit, as I walked around with Aaby, a mother holding a baby said she remembered him from when he visited her as a child some 30 years ago. His colleagues and assistants in the project affectionately call Aaby Homem Grande, which translates to “Big Man.”
Aaby has always been a bit of a lone wolf—he spends many days working by himself in his home office—but less so during the past 15 years. While Benn was in medical school in 1992 at Aarhus University in Denmark, she was advised to reach out to Aaby because she wanted to study whether vitamin A supplementation, routinely given with the measles vaccine in developing countries, interacted in any way with the vaccine. “I still have the piece of paper with his number,” Benn, who is 53, tells me as she sits on a bench in Aaby’s back garden, her arms hugging her legs. She has been working with Aaby ever since. Benn is now a professor of global health at the University of Southern Denmark and runs the Danish arm of the Bandim Health Project. She is prolific, having published more than 200 papers on issues that include the nonspecific effects of vaccines and the impact of vitamin A supplementation on infants in developing countries. She calls Denmark home but spends about 10 weeks a year in Guinea-Bissau. The two researchers bring to the field, and their relationship, complementary personalities: Benn, effervescent and philosophical; Aaby, serious and precise.
For the most part, Aaby and Benn’s work on the measles vaccine has supported Aaby’s original observations. In a landmark 1995 BMJ paper, they analyzed data from 12 previously published studies—some their own—on the association between measles vaccination and mortality in developing countries. They found that the vaccine was linked to a 30 to 86 percent reduction in overall death risk. In each study, measles itself killed only a small proportion of unvaccinated kids, so the vaccine wasn’t just preventing measles; something else was going on. In a 2014 paper published in JAMA, Aaby and Benn collaborated with Danish researchers to investigate whether these protective effects extended to high-income countries. They found that Danish children who received the live measles-mumps-rubella (MMR) vaccine as their last inoculation were 14 percent less likely to be hospitalized for any infection than were kids who had most recently received the inactivated DTaP-IPV-Hib vaccine for diphtheria, tetanus, acellular pertussis, polio and Hemophilus influenzae type B. This study inspired the 2017 analysis by the CDC that found live vaccines to be associated with even stronger protection in the U.S.
Aaby and Benn have also linked the BCG vaccine with lower neonatal mortality, and they have studied the live oral polio vaccine (OPV) as well. In a 2018 paper, they reported that child mortality rates were 19 percent lower after OPV campaigns than before them, and a clinical trial they published in 2015 found that OPV given within two days of birth with BCG reduced mortality risk by 42 percent, compared with BCG alone. Based in part on their findings, 15 scientists wrote a letter to the Lancet in 2016 arguing that the global switch from live OPV to IPV, the inactivated polio vaccine, which is part of a plan developed by the international Global Polio Eradication Initiative, could inadvertently increase child mortality.
The two scientists are certain that the evidence they have accumulated points to a clear conclusion: vaccines have more profound effects on the body than we thought. The big mystery they have been grappling with is how, exactly, all this happens.
A Broad Booster
Mihai G. Netea may have an answer. In 2010 Netea, an immunologist at Radboud University in the Netherlands, embarked on a study that he frankly didn’t think would be all that interesting. His laboratory was studying how the BCG vaccine affects human immune cells—how it teaches them to recognize and attack the bacterium Mycobacterium tuberculosis. To provide an experimental control on one test, lab workers exposed blood samples from vaccinated volunteers to Candida albicans, a common yeast. Based on accepted immunology doctrine, which holds that vaccines incite immune responses specific to the targeted pathogen, BCG should have had no effect on the blood’s response to Candida.
A few weeks later the student running the test approached Netea, concerned. “I think I did something wrong because I see differences with both tuberculosis and Candida,” Netea recalls her saying. Perhaps her samples had been contaminated; he suggested that she collect more blood samples and do the experiment over. She did, but the same thing happened. “She came again and said, ‘Well, I don’t know what to do, but I see precisely the same thing again,’” Netea says. He was flummoxed, so he started reading about BCG and found a handful of surprising animal studies that suggested the vaccine also protected some animals against malaria, influenza and Listeria monocytogenes, a common cause of foodborne illness.
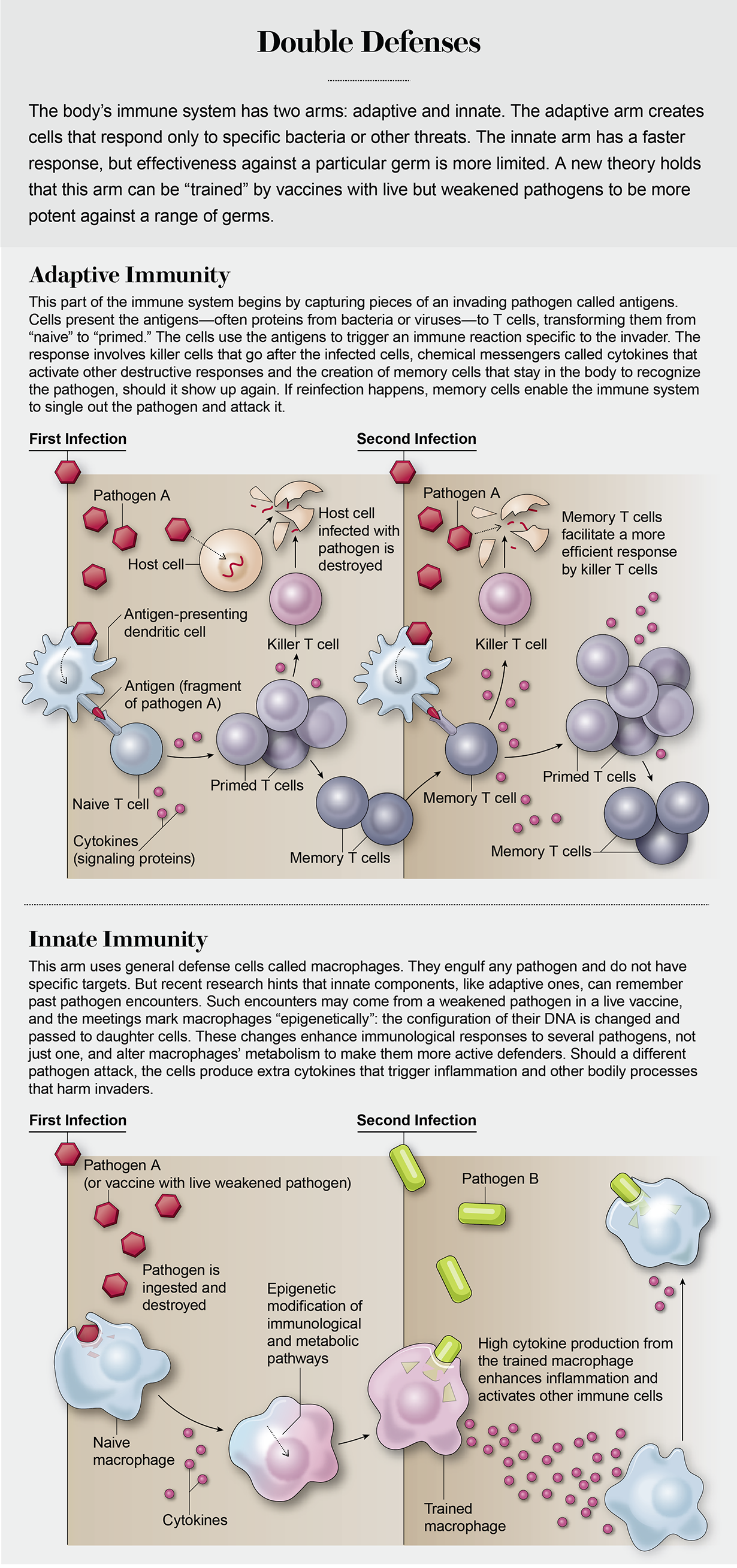
That is when Netea’s simple study transformed into a Greek siren, a creature beckoning for his full attention. How could a vaccine against tuberculosis change how the body responds to other pathogens? The idea contradicted established paradigms. Immunizations prime the body to make proteins called antibodies that recognize, attach to and attack proteins on the pathogens if the body ever encounters them again. This defense is called adaptive immunity, and it acts like a team of snipers that take out only certain targets. Given adaptive immunity’s specificity, it didn’t make sense to Netea that it could be responsible for BCG’s ability to protect against a number of insults.
Another kind of bodily defense—one that researchers historically thought vaccines had little to do with—is known as innate immunity, and it is more like a battalion told to open fire on anyone who edges into its line of sight. It is the rapid-response team, initiating a fight against any new invader. When pathogens invade, innate inflammatory cells get pulled to the infection site. Large white blood cells called phagocytes—particularly a type called macrophages—engulf and destroy the pathogens. They also secrete immune chemicals called cytokines that draw other immune cells to the scene. The reaction creates proteins that tag pathogens so that they are easier for phagocytes to find.
Given that BCG was increasing protection to multiple pathogens, it made sense to Netea that the innate immune system might be involved. But conventional thinking held that the innate immune system could not “remember” past immunological encounters, such as stimulation from previous vaccines. The thinking has long been that innate immune cells attack whatever they see and then forget about the battle afterward, like a soldier with amnesia. But these assumptions have been woefully incorrect.
In a paper published in 2012 in the Proceedings of the National Academy of Sciences USA, Netea’s team found that human immune cells primed by BCG produce four times as much of a key cytokine called IFN-gamma (IFN-γ) and twice as much of the cytokines TNF and interleukin-1 beta (IL-1ß) when later exposed to other pathogens. The cells can initiate these enhanced responses for as long as three months after vaccination, which suggests that the innate immune system can, in fact, remember what it learns. More recently, in 2018, the researchers reported that BCG reprograms human immune cells in ways that help them stave off the yellow fever virus.
Netea “has really pioneered a new field within innate immunology,” says Helen Goodridge, an immunologist at Cedars-Sinai Medical Center in Los Angeles. Studies by other labs also support his theory, showing that the measles vaccine boosts the body’s immune response to the toxin produced by tetanus bacteria, as well as its response when exposed to Candida.
It is unclear how the measles vaccine elicits its broad effects, but Netea’s work suggests that BCG trains the innate immune system by initiating changes in cellular metabolism and by shaping how key immune genes are controlled. After a person gets BCG, little molecular stamps are placed on important immune-related genes, and these stamps later identify the genes so that they can be quickly turned on when another pathogen invades. Why would a live vaccine elicit these effects better than an inactivated one? Researchers theorize that live organisms may stimulate a different reaction simply because they are alive—not just bits and pieces of an organism, as in the inactivated shots. (Real full-on infections, such as measles, do not seem to produce these advantageous effects and can actually suppress immunity.)

While wrapping up his 2012 study in PNAS, Netea stumbled across a trial that had just been published by Aaby and Benn suggesting BCG reduces general neonatal mortality—a finding that was criticized for being biologically impossible. Excited, Netea wrote to Aaby, telling him he had just discovered a mechanism that made sense of his findings. Since then, the two researchers and Benn have worked together to tease out the immunology behind the Guinea-Bissau data. Vaccines seem to “change the immune system, and they don’t just change it in the adaptive, pathogen-specific way,” says Tobias Kollmann, an immunologist and infectious disease physician at the University of British Columbia, who sometimes collaborates with Aaby, Benn and Netea. “They change it in all kinds of different ways.”
Trials on Trial
Neal Halsey agrees that Aaby has made important contributions to vaccine research over the course of his career—but his work on off-target effects is not one of them. Halsey, former director of the Johns Hopkins University’s Institute for Vaccine Safety, goes back a long way with the Danish scientist. He remembers that in the 1980s, Aaby was the first to identify a potential safety problem with a new, more concentrated measles vaccine introduced in Guinea-Bissau and other developing countries. At first, no one believed him—this appears to be a recurrent Aaby pattern—but then Halsey looked at data he had collected in Haiti and saw the same effects. Based largely on their findings, the WHO withdrew the vaccine from use in 1992.
But today Halsey thinks that Aaby is putting his convictions before the science. At the 2018 World Vaccine Congress in Washington, D.C., Halsey said the data from Guinea-Bissau may be real, but Aaby and Benn have been drawing causal conclusions from it that they shouldn’t. Kids who get vaccinated on time are often quite different from those who don’t: they can be healthier to begin with, or they can have wealthier parents with the means to drive them to the doctor and take better care of them in general. Concluding that vaccines are responsible for broadly different medical outcomes is too much of a stretch, Halsey says.
A 2017 BMJ study from the Netherlands illustrates his point. Researchers analyzed hospitalization rates among toddlers who had received a live vaccine as one of their last shots and then compared them with hospitalization rates among toddlers who had most recently gotten only inactivated vaccines. Scientists found that the live-vaccinated kids were 38 percent less likely than the others to be hospitalized for infections—but those children were also 16 percent less likely to be hospitalized for injuries or poisoning. Vaccines should not affect accident risk; the fact that the researchers found this link underscores the notion that vaccine history aligns with other factors in one’s life. The authors concede, though, that the way vaccines are administered in the Netherlands—they are scheduled in advance, and parents usually cancel appointments only if their kids are sick—most likely inflates the “healthy vaccinee” effect, as it is called, and findings from other countries may not be skewed so heavily.
Because it is so hard to interpret causality from observational studies, Halsey and others have called for Aaby and Benn to conduct more randomized controlled trials, the so-called gold standard for teasing out an intervention’s effects. In these studies, children are randomly selected to receive vaccines or placebos and then followed over time. This random allocation eliminates the chance that socioeconomic status or overall health will play a role in vaccine decisions. The problem is that vaccines are already recommended public policy around the world, so it is unethical for researchers to deny children vaccinations to study them. Thus, scientists must get creative—they have to design trials that provide children with extra vaccines or early ones, or they have to take advantage of natural delays in vaccine receipt.
To undertake a clinical trial in Guinea-Bissau is especially difficult. Aaby and Benn must store vaccines in a refrigerator at their house, where they have a generator, because the electrical grid is so unpredictable (they lost power every day during my visit). Political instability is another problem: one of their attempted trials was disrupted by a devastating civil war in 1998, in which Aaby also suffered a near-fatal wound when he was lanced by a piece of iron left behind by a thief who had looted his house. Some Bissau residents speak only rare dialects, which makes things difficult as well, and many don’t have phones.
Despite these challenges, Aaby and Benn are trying randomized trials, such as the one involving Maria. In a few completed tests, the results have not always supported their earlier findings. In a 2018 trial that Aaby and Benn worked on, for instance, researchers found that babies who got the recommended measles vaccine at nine months, plus an additional measles shot between four and 4.5 months, were no less likely to be hospitalized or to die than babies who did not get the extra doses. Yet the two are convinced the vaccine effects are real, just not fully understood. Halsey, though, finds their dogged persistence concerning. “Very good objective scientists acknowledge when an initial observation they made is shown not to be true,” he says.
Aaby and Benn are unpopular for another reason: they have published studies suggesting that inactivated vaccines, such as DTP, have detrimental effects, particularly for girls. Even though these vaccines protect against their targeted diseases, Aaby and Benn have linked these shots to a higher risk of other infectious diseases. It is unclear why this would happen—perhaps exposure to dead pathogens makes the immune system more tolerant of other future intruders—and critics argue the associations are not just spurious but also dangerous because they could further undermine the public’s confidence in vaccines. “Some of them just think that I’m a madman making trouble,” Aaby concedes.
A Search for Clarity
His battles, however, are entering a new phase. Although Aaby notes that his own research funds are running short, the WHO says that it will soon step into the arena. Aaby first contacted the agency about his findings in 1997; in 2013 it established a working group to review the data. In 2014 the WHO noted that the issue deserved further attention, and in 2016 and 2017 it discussed plans to oversee additional trials. One trial will investigate the effects on infant mortality of giving BCG vaccination at birth versus a placebo. The other will evaluate the effects of an extra dose of measles vaccine given with DTP between 12 and 16 months of age.
Aaby and others worry, however, that these trials will yield little clarity. The subjects will be given inactivated vaccines either at the same time as the live vaccines or after them, which, according to Aaby’s previous findings, could mute potentially beneficial effects. “We discussed this at length with many experts, and the evidence is clear that those trials will not give the answer,” Kollmann observes. Shann, the Australian pediatrician, agrees. These trials will be “a scandalous waste of time and money,” he says, because “none of those involved really understands the field.” And it is still unclear when the trials will start.
Ultimately Aaby worries that the WHO is just going through the motions. He suspects the agency wants to appear as if it is doing due diligence after its 2014 report on nontargeted effects but that its real goal is to make the issue go away. If nonspecific effects are real and powerful enough to save lives, then public health agencies will have to consider making changes to the vaccine schedule and perhaps even replace some inactivated vaccines with live ones, which would be extremely difficult.
In 2018 I asked Frank DeStefano, director of the CDC’s Immunization Safety Office, what it would take to make such changes in the U.S. “Certainly evidence would have to be stronger that this is a real effect,” he said. He noted that the agency had no plans at that time to collect more data on the issue. But even if it had additional evidence, he said, the CDC would have to consider all the possible risks and benefits before making policy changes.
Research in the field received renewed attention, however, early on in the COVID-19 pandemic, when scientists at more than 25 universities and clinical centers around the world began trials to test whether certain live vaccines, including the BCG vaccine and the oral polio vaccine, could reduce the risks associated with the coronavirus. Most of the trials are still ongoing.
The evening I left Guinea-Bissau I sat in the back garden with Benn, eating Danish cheese that she brought with her from her last trip home, and I thought about the couple’s philosophy of science. These researchers are not shy about their beliefs; they are convinced that nonspecific effects are real but so complex that many details remain a mystery, and they are not afraid to say so. To critics, this strength of conviction is a great weakness, a blazing preconception that biases their results. And it may do so. But bias is not unique to them. Scientists are people—people with ideas, and prejudices, and feelings—and every study involves interpretation. How do we know whose interpretations edge closest to the truth? Are those who admit to their beliefs more biased than those who don’t? Who should decide when enough evidence has amassed to reach a consensus, particularly when the implications are unexpected, inconvenient and consequential? Within this small and contentious field, at least, there are no clear answers.
“You have this feeling you are pulling a thread, and you don’t know how big the ball of yarn is,” Benn said to me. She was referring to the research on vaccines, but she could have been speaking about the scientific process itself. Biology is immensely complicated because our bodies are complex. The practice of science is complicated, too, because it is a product of humanity—an endeavor created and shaped by our imperfect minds. If vaccines do what Aaby and Benn think they do—and that is still an open question—it will take a lot more messy unraveling before the world sees things their way.