In just about any system or group, elements with a larger number of connections tend to have more clout than others. Think of Instagram “influencers,” for example—or the chief executive officers of companies.
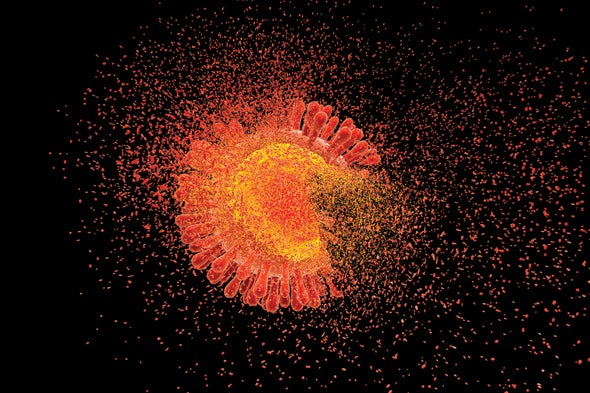
Even within a virus, some structural components—in this case, parts of proteins—have more links to one another than others do. And coaching the immune system to recognize and destroy such influencers is an efficient way to kill HIV, suggests a study published in May 2019 in Science.
There has been a lot of excitement in the HIV field since the March 2019 announcement that a second person, often referred to as the “London patient,” was cured after a bone marrow transplant. The donor carried a mutation that makes people naturally resistant to HIV; in effect, the procedure replaced the patient’s immune system with a new, resistant one. But bone marrow transplants are risky and invasive, and many experts believe a practical cure for the nearly 38 million HIV-infected people worldwide is more likely to come from smart molecular work. Most research done on HIV cures has so far focused on buttressing a person’s immune system. The Science study turns that approach on its head by looking for the most critical parts of the virus itself.
For this study, the researchers focused on “elite controllers”—people whose bodies control the virus without the aid of any drugs and who are estimated to number about one in every 300 infected individuals. It made sense that investigating how their immune systems kill HIV might point the way to a cure, says Bruce Walker, who is senior author of the paper and director of the Ragon Institute of Massachusetts General Hospital, the Massachusetts Institute of Technology and Harvard University. “There are not two people who are cured of HIV infection, in my view,” Walker says. “There are thousands—and a lot of them who control [the virus] on their own. We, as a field, need to pursue this with the highest priority.”
Walker and his colleagues found that elite controllers’ immune systems target the most influential regions in the virus. The researchers made this discovery by applying network theory, a type of analysis frequently used in mathematics to chart relationships between objects. They employed the theory to map connections between amino acids, the building blocks of proteins, in three-dimensional molecular structures of HIV proteins. (They used the 3-D structures because two amino acids that appear far apart in a protein’s linear sequence may be much closer—and connected—in three dimensions.)
The researchers found that some amino acids tend to have numerous branchlike structures that cause them to interact with many other amino acids. These branched amino acids have a high “network score,” Walker says, and are thus the most important to HIV’s integrity. HIV can mutate in a defensive response to a drug that targets a specific part of its structure. But the amino acids with high network scores are so important that the virus cannot vary them without great cost to itself: if those amino acids change, the connections are lost.
“If you take a highly networked [amino acid] and mutate it, the virus basically falls apart,” Walker says. “It dramatically loses fitness.” This finding makes such amino acids attractive targets for therapy because attacking them puts the virus in a lose-lose situation: it ends up destroyed whether it mutates or not. Walker’s team found that elite controllers’ immune systems tend to selectively target these influencer amino acids; in most other infected people, immune systems instead mount futile attacks on other, less important parts of the virus.
“This is impressive and important work,”comments Andrew McMichael, an emeritus professor of molecular medicine at the University of Oxford, who co-wrote a commentary accompanying the paper but was not involved in the research. “It explores why some [immune responses] are effective and why some are less effective.”
The research may also resolve some previously inconsistent findings about an immune molecule called B*57—which has been suggested as a magic weapon that elite controllers wield against HIV. B*57 is part of a group of molecules called human leukocyte antigens (HLAs), which make up a key part of the immune system. HLAs carry fragments of viruses to an infected cell’s surface so that killer immune cells circulating in the blood can recognize the flagged cell as infected and destroy both that cell and the virus within it.
There are thousands of HLA types, some more common than others, and some are better at controlling certain infections. Among these, B*57 is thought to be particularly potent against HIV. But scientists have been puzzled by the fact that not everyone with B*57 is an elite controller—nor do all elite controllers carry B*57. The new research suggests that what is key is not so much B*57 itself but the influencer amino acids that it targets.
B*57 “is the major determinant of progression or nonprogression [of HIV infection], but it’s not totally flawless,” McMichael says, adding that the 2019 paper “goes some way toward explaining why that may be.”
Walker and others have studied elite controllers for decades. One such person, Loreen Willenberg, now 67 years old, was diagnosed in 1992 and has since donated hundreds of samples for research. Willenberg, who says she has “an amazing immune system,” is invulnerable to dozens of pathogens, including HIV. Tests that measure her immune response to HIV still come back positive, but no test can detect the virus itself. “I’ve never measured a viral load, ever. It’s always been undetectable,” Willenberg says.
Walker had been following Willenberg’s health for about 15 years at the time of the study. But this time, instead of focusing on the aspects of her genetics that protect her from HIV, the team homed in on which parts of HIV her system attacks. “Here we don’t take into account host genetics at all,” Walker says. Yet the study still explains what makes her immune system so remarkable: it selectively attacks the amino acids with the highest network scores. “She fit the pattern perfectly,” he says.
With this confirmation of the importance of these influential amino acids, Walker says he hopes to develop a “therapeutic vaccine” that can be given to people already infected with HIV. The vaccine would contain about 30 of the viral parts with the highest network scores. The hope is that it would prime an infected person’s immune system to recognize and then go after these key targets and destroy the virus.
“We believe we can redirect the immune response,” Walker says. “We don’t know whether this will work, but there is a very strong rationale for it to do so.”