Magnetic resonance imaging (MRI) scanners are the most valuable diagnostic tool we have for assessing brain injuries and disorders. Yet around two thirds of people worldwide do not have access to MRI technology, and more than 90 percent of the devices are located in high-income countries. Expense is the big reason: a typical MRI machine costs around $1 million to $3 million. They need a purpose-built room to shield the scanner from outside signals and to contain the powerful magnetic fields generated by their superconducting magnets, which require liquid helium cooling systems that are pricey to run.
Low-cost, portable alternatives may soon start seeing widespread use. In a December 14 study in Nature Communications, researchers from the University of Hong Kong, led by biomedical engineer Ed Wu, describe an MRI scanner that needs no shielding and draws power from a standard wall socket. The approach, known as ultralow field (ULF) MRI, lacks the clarity and resolution required for precision diagnostics, but is much less expensive, with material costs under $20,000, the study authors estimate. What’s more, the machine’s design and algorithms are open-source, inviting researchers everywhere to help develop the technology.
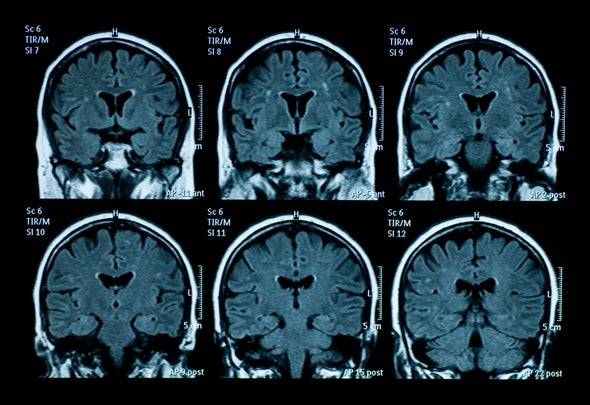
MRI exploits the fact that we are mostly made of water. The protons in hydrogen atoms have magnetically charged “spins,” which are aligned by the magnetic field and probed by radio-frequency pulses. Different tissues have distinct water concentrations and magnetic environments, and these differences appear as light and dark contrasts in reconstructed images.
Rather than superconducting electromagnets, the ULF design employs permanent magnets, thereby eliminating the need for cooling. The permanent magnets generate only 0.055 tesla, so no magnetic shielding is needed (standard MRI scanners use 1.5- or 3-tesla fields). The main trade-off is that the signals are weaker, so signal-to-noise-ratio is worse, and, as a consequence, image resolution is lower.
To maintain portability, the ULF design eschews physical RF shielding. Instead, the researchers used a “deep learning” algorithm trained to recognize and predict interference signals, which are then subtracted from the measured signals. “That’s one very useful innovation here,” says biomedical engineer Sairam Geethanath of Columbia University, who was not involved in the study. “It’s similar to noise-cancellation headphones, where you’re trying to learn the noise pattern in real-time and suppress it.”
The team demonstrated the device by scanning 25 patients and comparing the images with those from a standard MRI machine. The researchers could identify most of the same pathologies, including stroke and tumors. “The images appear of sufficient quality to be clinically useful in a number of scenarios,” says neuroscientist Tom Johnstone of Swinburne University of Technology in Melbourne, Australia, who was not involved in the study. “Rapid assessment of stroke, which has a large impact on success of interventions, could be facilitated by ULF MRI being located in more towns, or even mobile units.”
The new design joins a growing list of other ULF MRI scanners being developed. A company called Hyperfine, based in Guilford, Conn., received FDA approval last year for its portable scanner, but details of the design are proprietary. Wu and his colleagues have made their data, designs and code available online, which could speed ULF improvements and control costs. (Hyperfine’s machine is more than twice the estimated price of the Hong Kong team’s.)
Despite their promise, ULF devices are not intended to replace high-field scanners. They hold promise in “triage” settings, where patients cannot be moved or time is critical. “It has a role to play as an escalating device,” Geethanath says. The range of applications will likely grow as performance improves, and Wu has some ideas about this. “Right now, MRI systems are built as if we don’t know anything about what we’re scanning, but often the information we need is very subtle,” Wu says—namely, to identify what’s different. “That’s going to be a huge revolution, driven by cheap computing.” He envisions broader use of MRI technology, more closely matched to clinical needs at point of care. “The nuclear magnetic resonance phenomenon is a gift from nature,” he says. “We must use it more.”
A version of this article with the title “Portable View” was adapted for inclusion in the March 2022 issue of Scientific American.