It all began with a cough.
Four years ago Tracey McNiven, a Scottish woman in her mid-30s, caught a bad chest infection that left her with a persistent cough that refused to subside, even after medication. A few months later strange symptoms started to appear. McNiven noticed numbness spreading through her legs and began to feel that their movement was out of her control. When she walked, she felt like a marionette, with someone else pulling the strings. Over the course of two weeks the odd loss of sensation progressively worsened. Then, one evening at home, McNiven’s legs collapsed beneath her. “I was lying there, and I felt like I couldn’t breathe,” she recalls. “I couldn’t feel below my waist.” McNiven’s mother rushed her to the hospital where she remained for more than half a year.
During her first few weeks in the hospital, McNiven endured a barrage of tests as doctors tried to uncover the cause of her symptoms. It could be a progressive neurodegenerative condition such as motor neuron disease, they thought. Or maybe it was multiple sclerosis, a disease in which the body’s own immune cells attack the nervous system. Bafflingly, however, the brain scans, blood tests, spinal taps and everything else came back normal.
McNiven’s predicament is not uncommon. According to one of the most comprehensive assessments of neurology clinics to date, roughly a third of patients have neurological symptoms that are deemed to be either partially or entirely unexplained. These may include tremor, seizures, blindness, deafness, pain, paralysis and coma and can parallel those of almost any neurological disease. In some patients, such complications can persist for years or even decades; some people require wheelchairs or cannot get out of bed. Although women are more often diagnosed than men, such seemingly inexplicable illness can be found in anyone and across the life span.
Generations of scientists have tried to understand these bizarre conditions, which have historically been given diverse names, such as hysteria, conversion disorder or psychosomatic illness. These labels have, however, long imposed particular explanations for what many researchers now regard as a complex illness at the interface of psychiatry and neurology. Some are still in use today, but the newest name for these conditions, functional neurological disorder (FND), is deliberately neutral, simply denoting a problem in the functioning of the nervous system.
Patients with FND have long struggled to obtain adequate care. They have been accused of feigning or imagining symptoms, painfully but often fruitlessly probed for childhood trauma and dismissed by doctors who did not know how to treat someone who, based on all the usual tests, appeared to be healthy. “For many, many years physicians have underestimated the prevalence of these disorders and the human toll it takes,” says Kathrin LaFaver, a neurologist who specializes in movement disorders at Saratoga Hospital in New York State. “These people have really fallen [in the gap] between the fields of neurology and psychiatrynn.”
Over the past decade or so, however, using techniques such as functional magnetic resonance imaging (fMRI), researchers have begun to understand what happens in the brains of patients with this enigmatic illness. And by applying new models of how the brain works, they are gaining a better understanding of how the condition arises and how it may be treated.
Enigmatic illnesses
More than 3,000 years ago Mursili II, king of the Hittites, was caught in a terrifying thunderstorm. The experience left him with a temporary speech impediment that went away—only to return several years later, after the monarch woke from a nightmare about the incident. His subjects attributed their king’s curious ailment to the wrath of the Storm God, one of the most important deities of the ancient civilization. When modern-day scholars revisited the documents detailing the event, they interpreted it as functional aphonia (the inability to speak).
Like the Hittites, people throughout history have turned to the supernatural—gods, witchcraft and demonic possession—to explain illnesses that today would likely be diagnosed as FND. According to some historical interpretations, the first scientific attempt to account for them emerged around 400 B.C.E., when Greek physicians, including Hippocrates, coined the term “hysteria” to describe a wide collection of ailments, among them paralysis, headaches, dizziness and pain, in the belief that they were caused by the uterus (hystera, in Greek) wandering about the body.
Hysteria had its heyday in the 19th century, when it moved from the womb to the brain. Among several physicians who studied it was Jean-Martin Charcot, regarded by many as the “father of neurology.” At the Salpêtrière Hospital in Paris, he painstakingly detailed the symptoms of patients with hysteria and, after they died, conducted autopsies on their brains. Although Charcot was unable to identify any structural aberrations in those subjects, he was convinced that the impairments he saw were associated with unobservable, fluctuating changes in the brain, which he called “dynamic or functional lesions.”
Charcot also discovered that, contrary to common belief, male hysteria was not rare; instead it often went undetected. He highlighted, for example, cases of hysteria among workers at a national railway company that had seemingly emerged after minor physical injuries. His work popularized the study of hysteria, inspiring several researchers, including Joseph Babinski, Pierre Janet and Sigmund Freud, to investigate it as well.
Unlike Charcot, however, these men viewed the condition as a disorder of the mind rather than the brain. Freud proposed that it arose when repressed trauma from childhood abuse or other disturbing events was transformed into physical symptoms; accordingly, he called it conversion disorder. That view and label cemented the displacement of the disorder from the realm of neurology to that of psychiatry and became the dogma for much of the 20th century. Perhaps coincidentally, as Freud’s influence in psychiatry faded over the decades, so did cases of conversion disorder—to the point where some viewed it as a bygone ailment of the Victorian era.
A century later a new generation of investigators has turned its attention to this condition. Careful observation of patients indicates that despite the drop in diagnoses in the latter half of the 1900s, these disorders have not disappeared. And new research reveals that the condition encompasses both neurology and psychiatry. In 2013 some physicians, concerned that the term “conversion disorder” was not widely accepted by patients and perhaps incorrectly pointed to psychology as an exclusive driver for the condition, lobbied for a change—causing FND to be included as an alternative name for the ailment in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
Telltale Signs
On a cool, sunny afternoon in February 2020, I watched neurologist Jon Stone of the University of Edinburgh consult with first-time patients at the Anne Rowling Regenerative Neurology Clinic, where his team specializes in diagnosing and treating FND. Stone listened carefully as people described when, where and how their symptoms started. He collected detailed information about their medical and personal histories and conducted a neurological examination. Then, like a detective, he pieced these details together to make a diagnosis.
In recent years FND has gone from a diagnosis of exclusion—a label doctors reserved for patients whose conditions defied all other explanations—to one made after identifying distinct signs and symptoms. These resemble those of other neurological disorders but possess identifiable differences. One example is Hoover’s sign, in which weakness in a limb is temporarily corrected when the patient’s attention is directed elsewhere. Another is tremor entrainment: when patients with a functional tremor in one arm are asked to start shaking the other at a regular rhythm, the affected hand will start to shake with the same rhythm as the other. This effect does not occur in people with neurodegenerative conditions such as Parkinson’s disease. Clear signs of functional seizures include tightly shut eyes, rapid breathing and shaking that lasts for several minutes—features rarely seen during epileptic attacks.
Such indicators have been known to doctors for decades—Hoover’s sign, for one, was observed by physician Charles Franklin Hoover in the 19th century. In the past, physicians would hide such signs from patients, Stone explains. But he shows them to patients to help them understand the nature of their condition and notes that physicians are increasingly taking up this practice. Seeing such clues can help a person grasp a condition that Stone likes to describe as a “software problem, not a hardware problem” in the brain.
Stone first came across these disorders as a junior doctor in the early 1990s. He found himself fascinated by them; having grown up with a stutter meant that he had experienced being unable to control his own body. And he was disturbed by how those with FND, as he prefers to call the condition, were being treated. The common attitude among medical professionals was that the symptoms were not real—at least not in the same way as those seen in multiple sclerosis or stroke, for example. Many physicians were concerned that they would either fail to identify the true cause of a patient’s illness or be fooled by someone faking their symptoms. As a result, patients with FND did not receive the same level of sympathy, attention or care as those with so-called organic neurological illnesses.
Stone decided to dig deeper. During his doctoral studies at the University of Edinburgh, he met Alan Carson, who was training to become a psychiatrist and shared his interest. In 2002 the pair began to assess the scale of the problem by following the referrals to four neurology centers in Scotland over a period of 15 months. Their examination, which included more than 3,700 patients, revealed that 1,144—close to a third—had neurological symptoms deemed as partially or completely medically unexplained. Of those, only four ended up being diagnosed with another neurological issue 18 months after their initial consultation. This work demonstrated how widespread these disorders were.
Eventually Stone and Carson joined forces with Mark Hallett, a neurologist at the National Institute of Neurological Disorders and Stroke in the U.S., who had also been taking strides to advance the field. In addition to conducting his own research, Hallett had begun mobilizing a group of scientists and physicians who could contribute to the study of FND. The community gradually ballooned from several dozens of attendees at a small workshop to a full-blown society for FND, which was founded by Hallett, Carson and Stone and was inaugurated in 2019.
Predictions Gone Awry
A year after landing in the hospital because of her FND, McNiven was referred to a psychologist. At first, she did not think she needed to be there—her symptoms had been improving with physiotherapy. After several sessions of psychotherapy, however, McNiven made a shocking discovery: she had blocked the memory of certain key events in her childhood. Among those forgotten experiences were years of physical abuse at the hands of a family friend.
Although she had initially been reluctant to consider the role of psychological factors in her illness, McNiven now says that she thinks they do contribute. “I don’t think it’s just purely down to that,” she tells me. “But it certainly does have a big impact.” Many of those who study FND today would agree—with caveats. Unlike Freud, who focused on the role of repressed trauma, researchers now recognize that myriad factors are associated with this condition. These include predisposing factors, such as adverse experiences during childhood, a previous physical injury or mood and anxiety disorders; triggers such as physical injury or a stressful life event; and maintaining factors, such as a lack of access to proper treatment or a patient’s responses to and beliefs about the condition. The leading framework for thinking about FND, the so-called biopsychosocial model, takes all these factors into account.
As yet, there is no single, widely accepted explanation for how these influences come together to create FND, but some scientists have suggested that the malady involves arguably one of the most fundamental functions of the brain: predictive processing. Championed by neuroscientist Karl Friston of University College London, predictive processing posits that the brain is constantly making and evaluating predictions by comparing the data generated from our sensory organs to internal models built from previous experience. When mismatches occur between inferences and reality, the brain either updates its existing models or sends commands back down to the body to act in ways that align with our expectations. For instance, if you want to walk, but your leg is not moving, the brain will generate a prediction error that can be resolved if you move that leg. In this way, Friston and others propose, predictions underlie everything the brain does, from perception to movement to decision-making.
Neurologist Mark Edwards of St. George’s University Hospital in London and his colleagues have suggested that with FND, this predictive machinery goes awry, so that patients develop abnormal inferences of how their body should feel or function. One of the biggest drivers of this anomaly, according to Edwards, is excessive focus on one’s own body. This heightened attention can be attributed to a variety of factors, including an existing physical illness, mood and anxiety disorders, or childhood abuse. When a person experiences a triggering event—say, an injury to a limb or a panic attack—this heightened attentiveness may drive one’s brain to develop altered predictions about the body. In some cases, a past experience, such as exposure to sickness in the family, might also help shape these expectations.
Consider someone who falls and badly sprains a leg, resulting in a temporary loss of mobility in that limb. In most people, the brain’s predictions about the injured leg’s ability to move would get updated once mobility returns. This person, however, has a tendency toward mild anxiety that amplifies the levels of subconscious attention they pay to their body and has been sensitive to health events since the sudden death of a parent. These predisposing factors magnify the sensations associated with injury; in consequence, the internal model of the immobile leg persists even after the limb regains its function, leading to functional paralysis. (In some ways, this is the opposite of what happens in people who experience phantom limb syndrome. Those people are unable to update the prediction error that occurs when an expected sensation in a missing limb is not met with actual sensory feedback.)
The hypothesis that predictive processing is altered in FND patients has now been tested in a handful of experiments. In a 2014 study, for example, Edwards and his team used a task called force matching, in which a robotic device presses down on a finger and people are asked to match the force with their own hand. Healthy people tend to overestimate the force required by their own hand because the brain’s expectations “cancel out” some of its force (a similar explanation applies to why you cannot tickle yourself). People with FND, on the other hand, were abnormally accurate, indicating that the internal prediction system was functioning differently. Even so, much more evidence is needed to prove that this mechanism provides a correct and sufficient explanation for the condition.
Probing the Brain
Like Charcot, contemporary investigators of FND have been examining the brains of patients to find changes associated with the condition. Modern scientists, however, no longer have to wait to conduct an autopsy to peer into their subjects’ skulls. Using techniques such as fMRI, researchers have begun to reveal there are indeed differences in the brains of individuals with FND. “We’re beginning to identify the dynamic lesion that Charcot was looking for,” says David Perez, a neurologist-psychiatrist at Massachusetts General Hospital.
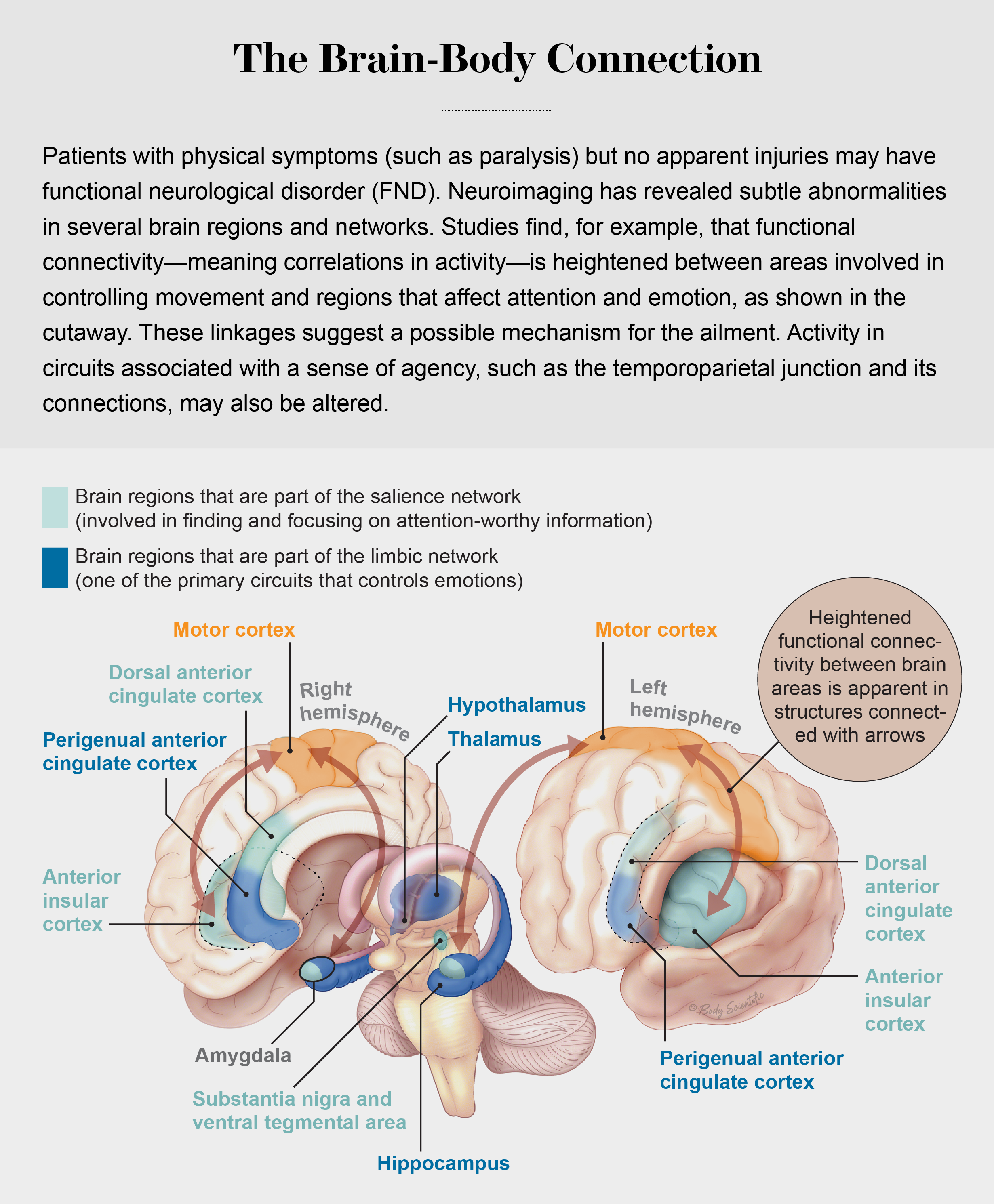
With fMRI, researchers have identified distinct patterns of activity in brain areas such as the temporoparietal junction—associated with a sense of agency—in those with FND, compared with those asked to mimic the same symptoms. These findings help to confirm that unlike conditions such as factitious disorder (a severe form of which is known as Munchausen syndrome), in which patients deliberately act out other illnesses, symptoms in individuals with FND are out of their control.
Another significant discovery from neuroimaging is that people with FND have enhanced connectivity between the motor-control regions and two brain networks involved in emotional processing: the salience network, responsible for detecting and focusing on attention-worthy information, and the limbic network, one of the primary systems controlling emotion. In a 2010 study, for example, s group reported Hallett’s group reported heightened linkages between the amygdala, a key region in the limbic system, and the supplementary motor area, which is responsible for preparing to initiate movements. Others, such as Perez, have shown hyperconnectivity between motor regions and salience network areas such as the insula and the anterior cingulate. These observations suggest that, at least in a subset of people with FND, the emotional circuitry might be hijacking the motor system, Perez explains.
Perez’s team has also found that some risk factors may map onto these circuits. In a study published in 2020, his group reported that the magnitude of the coupling of the motor regions with the limbic and salience areas of the brain positively correlated with the degree to which patients experienced physical abuse during childhood. Perez emphasizes, however, that this will probably be relevant only to the subset of patients in whom trauma is present: in his study, a significant proportion of patients did not report any childhood physical abuse. Still, he notes that these findings point to how a risk factor such as trauma could alter brain circuits in people who develop FND.
Scientists are also investigating how factors such as stress alter brain circuits in FND. Neurologist Selma Aybek of the University of Bern says that although not all patients have a history of trauma or stress, they may possess differences in their biological stress response. Her group has found that, compared with healthy individuals, FND patients have higher levels of the stress markers cortisol and amylase and report being more stressed after taking part in a stressful task. Building on these findings, her team is using neuroimaging to examine whether there is an association between stress-related regions and agency-related regions in FND patients’ brains.
Thus, a picture of the pathophysiology of FND patients is slowly emerging. But most of this work has been conducted in patients with motor symptoms, which means that sensory symptoms such as altered vision have yet to be explored. Many of these studies also have had small sample sizes, so findings will need to be validated in larger trials, says Valerie Voon, a neuropsychiatrist at the University of Cambridge, who collaborated with Hallett on several ground-breaking projects. How these neuroimaging findings fit with the predictive-processing model also remains an open question. It is plausible, Perez notes, that many of the areas identified so far may be the circuitry through which the altered predictions arise.
A Brighter Future
In the summer after her second year of teacher’s college in Scotland, a 19-year-old woman named Rachael Troup was rushed to the hospital with what appeared to be a stroke. Brain scans showed that she did not have a stroke, however, and tests for other neurological diseases came back normal. Eventually Troup was diagnosed with FND. But when she started treatment, it was excruciating. Neither her doctors nor her physiotherapists seemed to know much about how to treat her condition, and the exercises they made her do hurt more than they helped. “I was in pain constantly,” she says.
After a few months Troup decided to stop going to physiotherapy. At the time the entire right side of her body was barely functioning, and she was using a wheelchair for mobility. After being admitted to the hospital several more times for strokelike attacks, however, Troup met Stone’s team and was provided with FND-tailored care. It involved a form of physiotherapy that employs techniques such as distraction to shift the spotlight of attention away from the affected limbs while engaging in exercises to help restore normal control.
For FND patients, shifting focus away from affected limbs is often a crucial part of physiotherapy because, as Edwards’s predictive-processing model suggests, attention is critical to the generation of symptoms. With attention deployed elsewhere, the brain’s abnormal expectations about movement are unable to take hold. Stone and his colleagues are part of an ongoing U.K.-wide, randomized controlled clinical trial testing this type of specialized physiotherapy for functional motor disorders (a subset of FND affecting movement). In addition to retraining movement, the treatment includes educating patients about how such symptoms could arise and the physical and psychological factors that may underlie it.
To expand the tool kit of interventions for FND, researchers are also testing other alternatives. Another large clinical trial with more than 300 patients assessed the efficacy of cognitive-behavioral therapy (CBT)—a type of goal-oriented intervention focused on changing disruptive patterns of thinking or behavior—for functional seizures. The findings, published in June 2021 in Lancet Psychiatry, suggest that CBT may not reduce seizure frequency in all patients.
At King’s College London, neuropsychiatrist Tim Nicholson and his team are examining a noninvasive method of exciting the brain known as transcranial magnetic stimulation (TMS) as a potential intervention for FND. His group completed a feasibility study, and the results were promising enough for them to initiate a larger pilot clinical trial. There are competing explanations for why TMS might work. It induces a brief muscle twitch that could kickstart the relearning of movement; stimulating brain areas altered in FND might help restore function, or it may have a placebo effect. LaFaver, working with colleagues at Northwestern University, has examined the use of meditation and mindfulness practice, which, she says, patients have anecdotally reported as helpful for maintaining the benefits of treatment.
Psychological treatments such as CBT currently remain among the first-line interventions for people with FND, according to Perez. There is a pressing need for a range of effective treatments, however: the prognosis remains poor. It is still relatively uncommon for FND patients to completely regain function, and relapses occur often. According to a 2014 meta-analysis of 24 studies, on average 40 percent of patients reported similar or worsened symptoms seven years after their initial diagnosis. On top of that, patients still experience high levels of stigma and have trouble accessing treatment, LaFaver says. “I still think we have a long way to go.”
Fortunately, the situation is changing. As researchers’ interest in FND surged over the past decade, so did the number of FND clinics around the world. Patients are speaking up as well. In 2012, for example, the international charity FND Hope was established with the aim of raising awareness and empowering patients.
Still, debates linger—and are reflected in an ongoing tussle over the name of the illness. In what fraction of patients are psychological factors present, for example? Do symptoms primarily arise through conversion of stressors, or are other explanations also necessary? One meta-analysis found that reports of stressors in FND patients vary between 23 and 86 percent in different studies. W. Curt LaFrance, Jr., a neurologist-psychiatrist at Brown University, says that it takes more time to identify such stressors than some doctors can devote to an individual patient—which may account for this enormous spread. In his clinic and in the scientific literature, he has consistently seen evidence of psychological stressors having converted into physical symptoms, and, accordingly, he supports use of the term “conversion disorder.” Partially reflecting such views, the older name remained when FND was added to the DSM-5, but the need to identify psychological factors for a diagnosis was dropped. That excision also remains contentious.
One thing is clear, however: because the condition lies at the crossroads of neurology and psychiatry, insights from both fields will be necessary to solve the puzzle. This blurring of the line between mental and physical illness is a growing trend. Scientists now understand, for example, that stress—a psychological factor—can predispose people to Alzheimer’s disease and that inflammation—a physical factor—may give rise to depression. In addition, traditional neurological diseases such as epilepsy and stroke are often associated with mood and behavioral disturbances. “The brain doesn’t separate into neurology and psychiatry,” Perez says. “We need a new science of brain and mind that really encapsulates that brain health equals mental health and physical health.”
Over the past few years McNiven has frequently used a wheelchair because of her FND. But with the help of both physiotherapy and psychotherapy, she has started to recover. Her symptoms are not gone—she still experiences a lack of sensation in her legs, altered vision and pain—and some days are worse than others. “I constantly feel like I’m fighting against my body,” McNiven says. But she hopes to make a full recovery. “You’ve got to keep that positive attitude to keep fighting through it. There’s always hope you can get there with this condition.”