In her job as a physician at the Boston Medical Center, Sondra Crosby treated some of the first people in her region to get COVID. So when she began feeling sick in April 2020, Crosby wasn’t surprised to learn that she, too, had been infected. At first her symptoms felt like those of a bad cold, but by the next day she was too sick to get out of bed. She struggled to eat and depended on her husband to bring her sports drinks and fever-reducing medicine. Then she lost track of time completely.
For five days Crosby lay in a confused haze, unable to remember the simplest things, such as how to turn on her phone or what her address was. She began hallucinating, seeing lizards on her walls and smelling a repugnant reptilian odor. Only later did Crosby realize that she had had delirium, the formal medical term for her abrupt, severe disorientation.
“I didn’t really start processing it until later when I started to come out of it,” she says. “I didn’t have the presence of mind to think that I was anything more than just sick and dehydrated.”
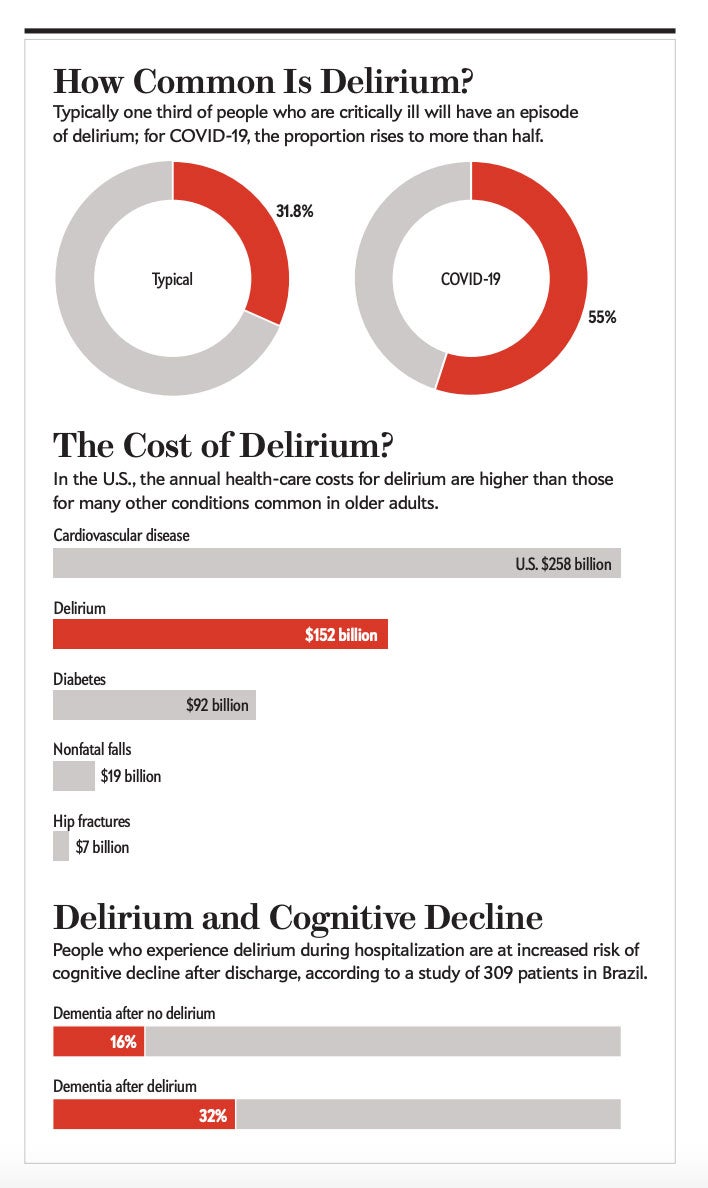
Physicians treating people hospitalized with COVID report that a large number experience delirium and that the condition disproportionately affects older adults. An April 2020 study in Strasbourg, France, found that 65 percent of people who were severely ill with the novel coronavirus had acute confusion—a symptom of delirium. Data presented at the 2020 meeting of the American College of Chest Physicians by scientists at the Vanderbilt University Medical Center showed that 55 percent of the 2,000 people they tracked who were treated for COVID in intensive care units (ICUs) around the world had developed delirium. These numbers are much higher than doctors are used to: usually about one third of people who are critically ill develop delirium, according to a 2015 meta-analysis [see “How Common Is Delirium?” in box below].
Delirium is so common in COVID that some researchers have proposed making the condition one of the disease’s diagnostic criteria. The pandemic has sparked physicians’ interest in the condition, says Sharon Inouye, a geriatrician at the Marcus Institute for Aging and Harvard Medical School, who has studied delirium for more than 30 years.
As clinicians face the immediate realities of confusion and agitation on their wards, Inouye and other researchers are concerned about the future. In the past decade long-term studies have revealed that a single episode of delirium can increase the risk of developing dementia years later and accelerate rates of cognitive decline in those who already have the condition. The reverse is also true: having dementia makes someone more likely to develop delirium. A set of simple steps, such as ensuring a family member is present to help people orient themselves, can reduce the incidence of delirium by 40 percent, but doctors struggle to follow that advice in COVID wards.
But the links between delirium and dementia have been difficult to untangle: researchers need to follow patients for years to get results. The surge in people with delirium produced by the pandemic has focused attention on the condition and provided scientists with a unique opportunity to follow patients and determine whether and how delirium might affect long-term cognition. Researchers have launched several studies to explore the long-term neurocognitive impacts of COVID, including dementia, and Inouye and others hope that this work will allow researchers to explore the links between the two conditions in real time.
If the pandemic can be said to have a silver lining, Inouye says, it has been to spur interest in how delirium can lead to dementia—and vice versa. What is more, says Catherine Price, a neuropsychologist at the University of Florida, the spread of COVID “has highlighted the blurring of the lines between delirium and dementia, especially with more older adults in our populace.”

Neglected condition
Inouye’s interest in delirium began when she landed her first job as an internal medicine physician at a Veterans Administration hospital in Connecticut in 1985. In her first month there, she treated more than 40 people for a variety of conditions. Six of them developed delirium during their stay; none seemed to return to their previous level of physical and mental health. To Inouye, the connection between her patients’ delirium and their poor prognosis was obvious. When she confessed her suspicions to her bosses, however, they just shrugged. Their attitude, Inouye says, was that delirium was just one of those things that happened.
“Why is it okay for older adults to come in the hospital and lose their minds?” Inouye asked. Answering this question, she says, would be “an uphill battle my entire career.”
Shortly after, she began a two-year fellowship to study the condition in depth. Her work showed that delirium occurs when several stressors converge. Preexisting vulnerabilities such as chronic disease or cognitive impairment can combine with precipitating factors, including surgery, anesthesia or overwhelming infection, to cause a sudden onset of confusion, disorientation and attention difficulties, especially in older adults.
“Delirium easily occurs when the brain is unable to compensate for a stressful situation,” explains Tino Emanuele Poloni, a neurologist at the Golgi Cenci Foundation near Milan, Italy. Researchers think that the underlying biological causes are inflammation and an imbalance in neurotransmitters—chemical messengers such as dopamine and acetylcholine.
Inouye’s mounting clinical experience has taught her that regardless of what precipitates delirium, around 70 percent of those with symptoms eventually recover completely. In the 30 percent who do not, however, an episode of delirium predicts a downward spiral over a period of months that leads to profound cognitive impairment or even to symptoms of dementia.
More formal studies have reinforced the link, to varying degrees. Inouye investigated a group of 560 people aged 70 or older who had undergone surgery, and she saw that cognitive decline over the subsequent 36 months was three times faster in those who developed delirium than in those who did not have the condition. A 2020 meta-analysis of 23 studies showed that delirium during a hospital stay was associated with 2.3 times greater odds of developing dementia. And work by a team of Brazilian scientists showed that in a group of 309 people with an average age of 78 years, 32 percent of those who developed delirium in the hospital progressed to having dementia, compared with just 16 percent of those who did not become delirious [see “Delirium and Cognitive Decline” in box below].
What is more, the longer a person is delirious, the greater their risk of subsequent cognitive impairment, according to a 2013 study by psychologist James Jackson of Vanderbilt and his colleagues. Work by Inouye, Jackson and other researchers found that the reverse was also true: even after controlling for age, existing dementia symptoms increased the chances of developing delirium.
Causing confusion
Scientists still do not agree on whether the link between delirium and dementia is strong only in those who would have developed dementia anyway or whether delirium increases the risk of cognitive decline even in individuals who are not predisposed to it. Nor can they say precisely what it is about delirium that may provoke dementia. If researchers could identify these connections, then perhaps they could prevent delirium from escalating into dementia.
“We don’t understand the mechanisms of delirium at all—we really don’t. And there is no successful management of delirium from a pharmaceutical standpoint,” Price says.
Scientists have developed three hypotheses to explain how delirium might provoke dementia. One line of thinking holds that an accumulation of toxic cellular trash in the brain could cause short-term delirium and lead to longer-term damage. The body usually clears this molecular rubbish by way of the bloodstream and the glymphatic system, which is a network of channels filled with cerebrospinal fluid. Damage to vessels from an acute episode of delirium could persist and trigger dementia, or a brain that experiences delirium could become more prone to vascular problems in the future.
The second suspect is inflammation, which often troubles people who are hospitalized for infections, respiratory distress or cardiovascular disease. Surgery and severe infections can cause a buildup of cellular detritus in the brain, which triggers more inflammation. This short-term, all-hands-on-deck reaction safeguards the brain because it clears the harmful debris, and the inflammation ultimately dies down. That is not the case for those who develop delirium, Inouye says. Persistent inflammation can trigger an acute episode of delirium and cause neurons and associated cells, such as astrocytes and microglia, to deteriorate, leading to cognitive damage.
The third idea is what is referred to as the threshold hypothesis. Someone with dementia (even in the earliest stages) has fewer connections between neurons and can show damage to the insulation that wraps them and helps to convey signals, known as white matter. This loss strips the neurological reserves that help the person to cope with inflammation or infection, throwing them over the edge not just into delirium but into a more advanced dementia.
Even though the genesis of delirium and its molecular connections to dementia remain unknown, Inouye has managed to find a way to cut rates of delirium in hospitals. She created a program of simple strategies known as HELP (Hospital Elder Life Program), which focus on reducing sedation even during mechanical ventilation, paying close attention to nutrition and hydration, and ensuring the presence of family members to help reassure and orient patients. A 2015 meta-analysis showed that these steps reduced delirium by around 40 percent. Hospitals around the U.S. began instituting these simple protocols. Then COVID struck and made them all but impossible.
Dementia surge
As Crosby endured coronavirus-induced delirium in her Boston bedroom, Poloni was treating delirious people with COVID in Lombardy—Italy’s ground zero for the coronavirus. Many of Poloni’s patients already had dementia, and like many physicians, he was watching for common symptoms of respiratory infections such as fever, cough and difficulty breathing. But some of his patients did not show those signs at all. Instead they mostly became “dull and sleepy,” Poloni says. Others became restless and agitated—all signs of delirium. It was so prominent that Poloni argued that delirium should be added to the virus’s diagnostic criteria. Inouye has made that argument, too, and it is supported by a study she published in October 2020 showing that 28 percent of older adults with COVID have delirium when they present to the emergency department.
The high numbers of people who developed delirium immediately made Inouye, Price and other researchers worry that the pandemic could lead to a surge in dementia cases in the coming decades, on top of the increase in cases as a result of aging populations [see “The Cost of Delirium?” in box above]. “Is there going to be an increase in dementia from people who had COVID during adulthood or midlife?” asks Natalie Tronson, a neuropsychologist at the University of Michigan. “What happens over the next decades as the population ages more?”
In a concerted effort to find answers, institutes around the world have funded a variety of studies into the long-term cognitive effects of COVID, some of which look at delirium. One such study in the U.S. tracked people who were treated in the hospital for COVID, many of whom developed delirium during their stay, and measured their cognitive and psychiatric function. An international study is planned to measure the prevalence of delirium in patients with COVID in ICUs, as well as identifying factors that predict long-term outcomes.
A separate study in Germany and the U.K. is also tracking neurocognitive outcomes in people with COVID to determine how delirium affects brain function months later. Another research project led by a team at Vanderbilt is looking for an alternative to commonly used sedatives such as benzodiazepines, which are known to increase delirium. The researchers are testing a sedative called dexmedetomidine to evaluate whether it is a safer option for people who are hospitalized with COVID.
Inouye and Tronson hope that the funding of these long-term studies will lead to ongoing scientific interest in the delirium-dementia connection—and provide some insight.
“It’s going to be, I think, a little bit frightening and a little bit enlightening about how illness affects dementia risk but also about what other lifestyle and genetic protective factors can influence risk as well,” Tronson says. “We’re learning quickly, but there are still a lot of black boxes.”
This article is reproduced with permission and was first published on December 02 2020.



