Shortly after the end of the Second World War, large numbers of wealthy businessmen in the United States began dying from heart attacks. Shocked by the obituaries mounting up in his local newspaper, physiologist Ancel Keys decided to investigate. His findings would fundamentally change the way we eat for decades to come.
Keys couldn’t understand why high-powered US executives, with access to plentiful food, had much higher rates of coronary heart disease than did people in post-war Europe, where food shortages were common. Then it dawned on him: could there be a correlation between fat in the diet and heart disease? Keys presented his diet–heart hypothesis with gusto at a World Health Organization meeting in 1955. Six years later, his face appeared on the cover of Time magazine, in which he urged readers to shun fatty foods such as dairy products and red meat.
Keys’ Seven Countries Study, launched in 1958, explored the diet, lifestyle and incidence of coronary heart disease in nearly 13,000 middle-aged men in Finland, Greece, Italy, Japan, the Netherlands, the United States and Yugoslavia1. The findings showed that blood cholesterol levels and heart-attack death rates were highest in countries with diets high in saturated fat, such as the United States and Finland. Around the time that Keys was setting up his trial, the Framingham Study2 of more than 5,000 residents of a Massachusetts town identified high cholesterol as a major risk factor for coronary heart disease.
Landmark studies such as these laid the groundwork for the introduction of dietary guidelines in the United States and the United Kingdom during the 1970s and 1980s. The recommendations advised citizens to reduce their consumption of saturated fat to about 10% of their total energy intake, to lower cholesterol in the blood and therefore decrease the chances of a heart attack. In the public consciousness, a low-fat diet has been synonymous with good health ever since.
But not everybody agrees. Uffe Ravnskov, a Danish independent researcher based in Lund, Sweden, dismisses the relationship between dietary fats, cholesterol and coronary heart disease, calling it “the greatest medical scandal in modern time”. Critics such as Ravnskov say data points in Keys’ Seven Countries Study were cherry-picked to fit the conclusion. For instance, Keys did not include data from France, where the occurrence of heart disease was comparatively low at the time despite the nation’s high-fat diet. Ravnskov’s The International Network of Cholesterol Skeptics, which has around 100 members—some of them cardiologists—says millions of people have been “badgered” into eating a “tedious and flavorless diet” out of fear for their hearts.
Cholesterol confusion
Robert DuBroff, a cardiologist at the University of New Mexico in Albuquerque, used to take the theory linking lipid in the diet with heart disease as gospel. But around 15 years ago, he noticed editorials critiquing the dogma were cropping up in the scientific literature. The debate prompted him to revisit the Framingham Study. He was surprised to find that the cholesterol levels of those who developed coronary heart disease and those who did not were pretty much the same, except when total cholesterol was either exceptionally high (more than 380 milligrams per decilitre) or low (less than 150 milligrams per decilitre). “For the vast majority of patients in the middle, cholesterol levels really did not distinguish those who did or did not develop heart disease,” DuBroff says.
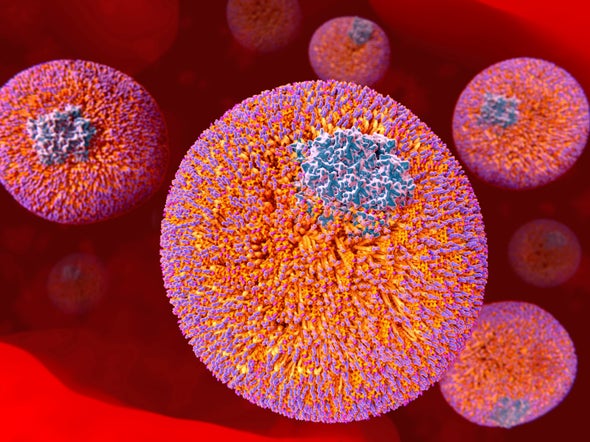
When cholesterol is implicated in causing cardiovascular problems, it is not the lipid itself that is the culprit, but rather the lipoproteins that carry cholesterol to and from cells. Broadly, these can be categorized into two groups: high-density lipoprotein (HDL), colloquially referred to as good cholesterol; and low-density lipoprotein (LDL), or bad cholesterol, that clogs arteries and increases the risk of heart attacks. This distinction was determined in the 1950s by US physician John Gofman. His experiments analysing the blood plasma of people who had had a heart attack found big increases in the levels of LDL, whereas HDL levels were lower than normal. The cholesterol theory gained widespread acceptance in 1984, when a trial of around 3,800 people found that those with lower levels of LDL had a reduced risk of having a heart attack or of needing bypass surgery3.
The link between LDL and heart disease is indisputable, says Jane Armitage, an epidemiologist at the University of Oxford, UK. As evidence, she points to studies of people with familial hypercholesterolemia—a condition that arises from a mutation in the gene encoding the LDL receptor protein. This protein usually removes LDL cholesterol from the blood, but in people with the condition it is faulty. As a result, people with familial hypercholesterolemia have abnormally high levels of LDL cholesterol and, if left untreated, are up to 13 times more likely to develop coronary heart disease than someone without the mutation.
The advent of statins—medication that lowers LDL by inhibiting a cholesterol-producing enzyme in the liver—reinforced the view that LDL cholesterol has a substantial role in heart disease. In the early 1990s, the Scandinavian Simvastatin Survival Study showed that the statin simvastatin was effective at lowering LDL cholesterol and reducing the risk of a heart attack4. Since then, numerous randomized clinical trials have shown that statins reduce heart attacks, strokes and death. A review in 2016 concluded that, for every 10,000 people with vascular disease, a daily statin would prevent 1,000 heart attacks, strokes and coronary artery bypasses5. “For people to doubt that statins save lives in high-risk people seems to be just extraordinary in the light of the very strong evidence,” says Armitage.
Some researchers, however, still have their doubts. DuBroff argues that the substantial body of evidence supporting statins has never been properly validated. His systematic review of published clinical trials comparing several cholesterol-lowering drugs with placebos found that the medications did not necessarily reduce the risk of death6. And although most specialists broadly consider the evidence for statins to be strong, the same can’t be said of cholesterol-lowering drugs with different mechanisms of action, such as fibrates and ezetimibe, he says. “If this concept of lowering cholesterol is valid,” he asks, “then why aren’t these other agents equally effective at reducing cardiovascular events?”
Fat or fiction
Armitage insists that the cholesterol theory is scientifically sound, but she admits it is difficult to draw direct conclusions about heart disease from dietary studies. In gold-standard randomized controlled trials, people replace saturated fats in their diets with polyunsaturated fatty acids, such as those found in vegetable oil, and this reduces the levels of LDL cholesterol in the blood. But, curiously, most trials have failed to show a mortality benefit. Many other dietary studies looking at heart disease are observational and rely on participants completing a food questionnaire from memory—a method that has its limitations. “Such approaches give a general indication of the types of food that are associated with heart disease,” says Tim Chico, a cardiologist at the University of Sheffield, UK. However, “an association doesn’t prove that there is a causal link”, he adds.
This swirl of contradictory findings could indicate that the perils of eating saturated fat have been overstated, and that other dietary components that contribute to the pathogenesis of heart disease might have been overlooked. Four years before Keys appeared on the cover of Time, British physiologist John Yudkin floated the idea that the real danger to public health was sugar. His findings were largely ignored at the time. In 2016, however, it was revealed that influential research in the 1960s that had downplayed the role of sugar in coronary heart disease had been funded by the sugar industry7.
Shortly after this revelation, results from the PURE (Prospective Urban Rural Epidemiology) study suggested that diets high in carbohydrates, not fats, are the ticket to an early grave. The study found no association between high fat intake and the occurrence of heart attacks or cardiovascular disease8. Moreover, it suggested that diets high in saturated fat actually reduced the risk of stroke by roughly 20%. “Emerging data are showing us that refined sugars are likely the main culprits in our diet, not fat,” says lead researcher Mahshid Dehghan, a nutritionist at the Population Health Research Institute in Hamilton, Canada. But PURE was an observational study that relied on questionnaires, and so had the same limitations as many other nutritional studies.
DuBroff stops short of calling himself an all-out cholesterol sceptic, but he is convinced that placing the blame on bad cholesterol gives, at best, a partial picture. “Focusing just on LDL is an oversimplification of a very complex disease process,” he says. He points out that research co-authored by Ravnskov found that people with the highest level of LDL cholesterol seem to live longer than those with the lowest levels9. And research in 2019 suggested that levels of a particular subclass of LDL might be a better predictor of heart attacks than is the total amount of LDL present10. Clearing up the confusion about the effect of cholesterol, DuBroff says, will require more research into other biochemical mechanisms and dietary components that could cause heart disease, such as insulin resistance and inflammation.
Despite critics poking holes in his most famous work, Keys’ lifestyle seemed to have worked for him. He died in 2004 at the age of 100, having followed a Mediterranean diet (rich in olive oil, starchy foods and vegetables, and low in saturated animal fat) for most of his life. This is the plan Chico recommends for his patients. He’s not fussed if they want to forgo the pasta and also make the diet low in carbohydrates. “Why does it have to be an either–or?” he says. “I would very much like to see a more constructive discussion about how we tackle the multiple influences of heart disease, rather than a popularity contest between one or the other.”
This article is part of Nature Outlook: Heart health, an editorially independent supplement produced with the financial support of third parties. About this content.
References
-
Keys, A. (ed.) Circulation 41, S1–S211 (1970).
-
Kannel, W. B., Dawber, T. R., Kagan, A. & Stokes, J. Ann. Intern. Med. 55, 33–50 (1961).
-
The Lipid Research Clinics Coronary Primary Prevention Trial. J. Am. Med. Assoc. 251, 351–364 (1984).
-
Scandinavian Simvastatin Survival Study Group. Lancet 344, 1383–1389 (1994).
-
Collins, R. et al. Lancet 388, 2532–2561 (2016).
-
DuBroff, R., Malhotra, A. & de Lorgeril, M. BMJ Evid. Based Med. https://doi.org/ghzn8g (2020).
-
Kearns, C. E., Schmidt, L. A. & Glantz, S. A. JAMA Intern. Med. 176, 1680–1685 (2016).
-
Dehghan, M. et al. Lancet 390, 2050–2062 (2017).
-
Ravnskov, U. et al. BMJ Open 6, e010401 (2016).
-
Hua, J. & Malinski, T. Int. J. Nanomed. 14, 8973–8987 (2019).