The body’s constellation of gut bacteria has been linked with various aging-associated illnesses, including cardiovascular disease and type 2 diabetes. Now a study has found that aging itself is associated with microbiome changes, and that these alterations are distinct from those connected to diseases or medication use. The findings raise the possibility that shifts in gut bacteria help drive the aging process—and that protecting these microbes could help people lead longer, healthier lives.
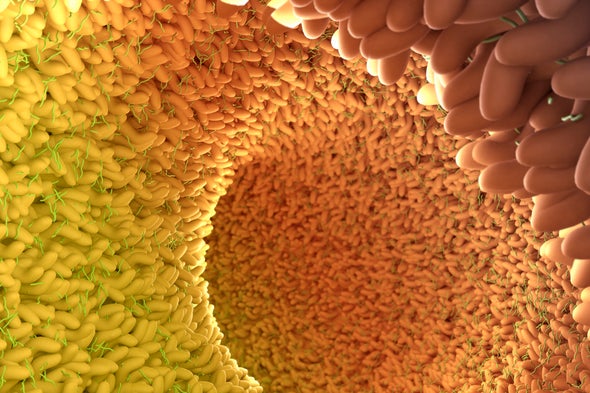
In the new study, published in Cell Reports on September 28, researchers at Cedars-Sinai Medical Center in Los Angeles sampled bacteria from the small intestines of 251 people between the ages of 18 and 80 who were undergoing upper endoscopies, when a doctor sticks a small probe down the throat and past the stomach. Usually, researchers study gut bacteria through stool samples. But those microbes, coming from the very end of the bowel, can be quite different from bacteria in the small intestine, closer to the stomach. That’s where most digestion and nutrient absorption occurs. “All the magic happens in the small intestine,” says study co-author Mark Pimentel, a gastroenterologist at Cedars-Sinai.
After analyzing the samples, the researchers found that aging was linked with changes in bacterial populations. Older people had more bacteria from the families Enterococcaceae, Lactobacillaceae, Enterobacteriaceae and genus Bacteroides, “and those are all groups of bacteria that can cause disease in humans,” says Heidi J. Zapata, an infectious disease specialist and immunologist at the Yale School of Medicine, who was not involved in the study. E. coli bacteria, which belong to the Enterococcaceae family, for instance, can cause diarrhea and urinary tract infections. Overall bacteria diversity also declined as people got older, going down as people headed towards age 80. Low diversity has been linked to health problems too, Pimentel says. Studies have found a relationship between low bacterial diversity and Crohn’s disease, irritable bowel syndrome and colorectal cancer, among other conditions.
It is not crystal clear how changes to the microbiome might drive aging, or if they really do. Research in rodents has shown that disruptions to gut bacteria can make it harder for intestinal stem cells to regenerate. This could affect metabolism as well as the overall health of the intestinal barrier; problems with that barrier have been tied to aging and age-related conditions such as liver disease, metabolic diseases, inflammatory bowel diseases, and lung and brain problems. The microbial changes that occur later in life may also create a more inflammatory environment in the gut, helping to drive the aging process. When researchers transplanted gut microbes from older mice into younger germ-free mice in a 2017 study, the young mice developed inflammation that is indicative of aging.
Because the new study only found associations, it does not prove that these changes cause aging. Instead, gut bacteria might change after people get older. “We really don't know the chicken or the egg here, but we need to find out,” Pimentel says. He hopes to tease out answers in future studies, including additional experiments that transplant “older” microbiomes into young animals to see if it makes them age faster or become ill. It would also be interesting, he says, to study the microbiomes of healthy centenarians and identify differences that could play a role in healthy aging.
It’s also unclear just how broadly applicable the new findings are, though, because the patients were undergoing upper endoscopies—and “endoscopy is not something people happily volunteer for,” says Elena Biagi, a researcher who studies the microbiome at the University of Bologna in Italy, who was not involved in the study. These people may have had underlying medical issues that prompted them to get endoscopies, so their gut bacteria may not have been representative of normal, healthy individuals.
The researchers were also able to figure out that medication use and the presence of disease affected the small intestine microbiome, separate from aging. They found, for instance, that the more medications people took, the more Klebsiella bacteria they had in their intestines—but that the abundance of Klebsiella was unrelated to their age or the number of diseases they had. Klebsiella can cause hospital-associated infections including pneumonia, surgical site infections, and meningitis, and these bacteria are often antibiotic-resistant. They also found that people with underlying conditions, regardless of their age or medication use, tended to have more Clostridium bacteria in their intestines, which can cause dangerous C. difficile infections.
If, in future studies, researchers do show that microbial changes drive the aging process rather than the other way around, then protecting the microbiome through healthy lifestyle choices or targeted medical interventions may keep people healthier for longer. Pimentel says eating well and exercising almost certainly help. Zapata encourages people to also be judicious in their use of antibiotics—to avoid taking them when they aren’t needed, and to take targeted antibiotics rather than drugs that kill off a broad array of bacteria. After treatment with broad-spectrum antibiotics, gut bacteria tend to grow back with less diversity, she says, and more unhealthy kinds of bacteria can thrive.
“An unbalanced microbiota can definitely lead to infections and disease,” she says. “It is important to understand these changes that happen as we get older to try to see if we can improve the aging process.”