As the novel coronavirus swept through Boston last March, Toni Choueiri was worried. He was concerned not only about the rapid rise in COVID infections but about the swift shutdown in cancer screenings.
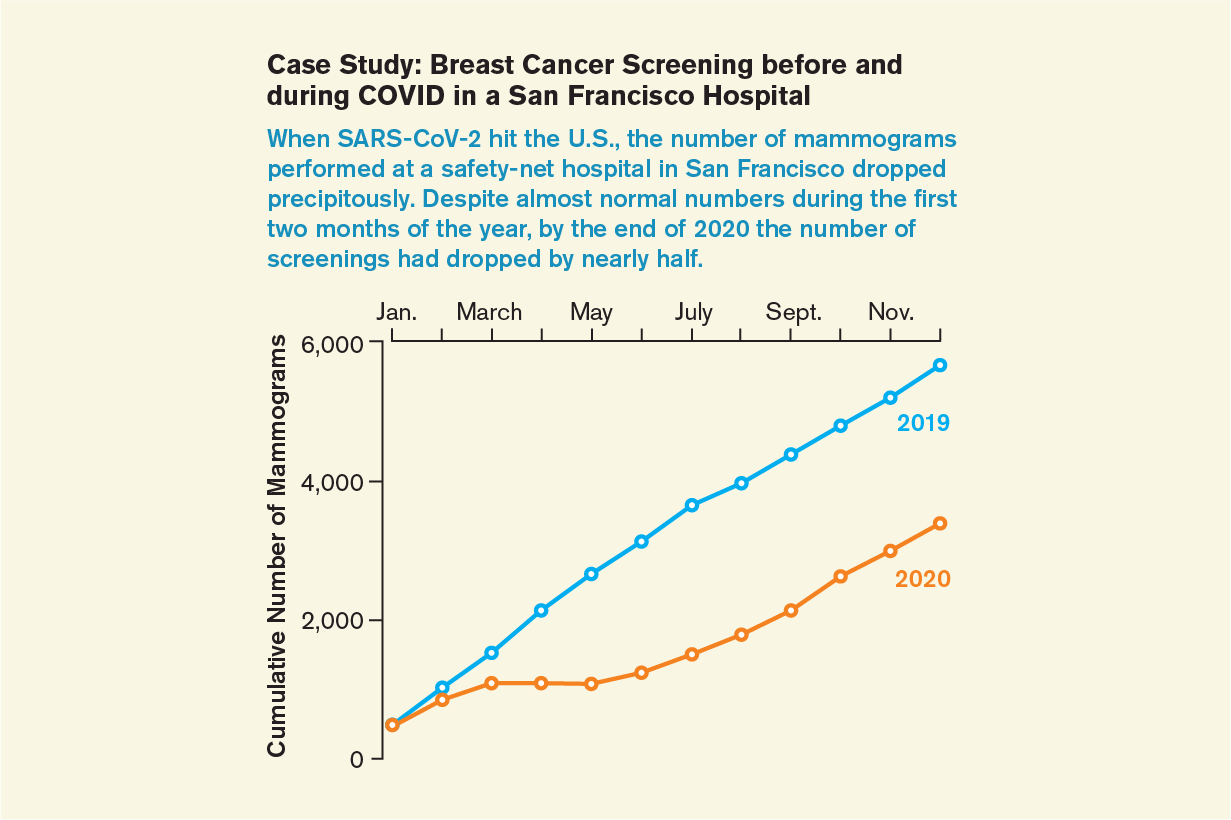
In Boston—and around the nation—colonoscopy suites stood empty as patients refused to come in, terrified of setting foot in any hospital or clinic. Screening center schedules, once full of mammography appointments, cleared dramatically. Hospital corridors quieted; screening center workers were sent home. Hospital administrators struggled to find enough PPE to take care of urgent surgeries, and elective procedures fell to the wayside. As COVID cases surged frighteningly across the country, cancer detection seemed to be the last thing on anyone’s mind.
Choueiri, who directs the Lank Center for Genitourinary Oncology at the Dana-Farber Cancer Institute, saw a steep drop in new consultations in the pandemic’s early months. The veteran oncologist feared that the lack of screenings, which aim to detect cancer at its earliest stages, would lead to a tidal wave of missed diagnoses. He worried about tumors seeding, taking hold, growing and metastasizing without being detected. He envisioned a future with streams of patients who had cancers so advanced he could no longer cure them.
Driven by these concerns and a desire to know exactly how bad the problem was, Choueiri and his colleagues turned to the data. Their study, published in JAMA Oncology in January 2021, showed a steep drop in screening from March to June of 2020 in his health system, Massachusetts General Brigham. More than 60,000 patients are typically screened there for cancer in a three-month period; in the first three months of the pandemic, he says, fewer than 16,000 came in for tests. In those early days National Cancer Institute officials estimated the pandemic would result in 10,000 excess cancer deaths in breast and colon cancer alone over the coming decade.
Screenings for some cancers fell by 90 percent when COVID struck, making a postpandemic surge of cancer deaths seem a foregone conclusion. As the pandemic wore on, some cancer centers began to report a worrisome increase in advanced cancer diagnoses. But as more time passed and screenings resumed, the outlook grew less dire. COVID may prove to be a grand experiment assessing the import of cancer screening, and results are beginning to trickle in. But because both the disease and its epidemiology are so complex, those results may take years, or even decades, to become clear.
Skipped Screenings
One patient whose pandemic screening turned up early-stage breast cancer was Senator Amy Klobuchar of Minnesota. After delaying the procedure, she had a routine mammogram in February 2021. With surgery and radiation completed and a good prognosis in hand, Klobuchar is urging others not to put off their screenings. “I hope my experience is a reminder for everyone of the value of routine health checkups, exams and follow-through,” she wrote in a recent blog post.
Cancer kills some 600,000 people in the U.S. every year. Screening tests such as Pap smears, mammograms, colonoscopies, lung scans and prostate-specific antigen tests clearly save lives: although rates vary by cancer type, five-year survival is consistently higher when the disease is caught in its early stages. Yet as the pandemic spread throughout the U.S. and the world, rates of those routine screenings fell precipitously. This was especially true for colonoscopies, the most invasive screening and an exam that many avoided even before the pandemic. Choueiri’s health system usually performs more than 9,000 colonoscopies in any three-month period; in March, April and May of last year, there were just over 1,700 in total. Similar drop-offs were seen across the country, where in some cases up to 95 percent of colonoscopies were missed in the first months of the pandemic.
Screening rates synchronized with pandemic waves, bouncing back in the summer of 2020 before falling during subsequent surges. Those who never rescheduled may be up to two years behind. “Between the peaks, what we didn’t see was sufficient recovery,” says Karen E. Knudsen, chief executive officer of the American Cancer Society. “We’ve made progress getting people back in the door, but there’s a large population that is underscreened. We don’t know the impact of this yet, but it’s definitely a problem.”
One major issue, Knudsen says, is that people who miss screenings aren’t always flagged for follow-up. And some tests, such as those for prostate cancer, are harder to track using medical records because of how they are coded. In fact, she says, determining how many people are overdue for screening is virtually impossible because of the diverse settings in which patients receive screenings and because there is no national infrastructure that tracks them in real time. “We don’t know who didn’t come back,” Knudsen says.
According to a study published in JAMA Oncology in April, nearly 10 million people missed screenings for breast, colon and prostate cancer between March and May of 2020, but no one knows how many of those tests remain unscheduled. Those who missed screenings, Knudsen says, are likely to be people who haven’t been screened before, because they either just became eligible during the pandemic or were already hesitant. “We can infer that hesitancy is only enhanced with COVID,” Knudsen says.
Tracking Missing Patients
Coaxing overdue patients into a clinic is one of Rachel Issaka’s primary concerns. Issaka, a gastroenterologist and assistant professor at the Fred Hutchinson Cancer Research Center and University of Washington, says it is critical that health systems track down these missing patients. A study she published in June found that hundreds of colonoscopies were canceled between March and May 2020, and more than half of those people had not yet returned. Of those who did, more than 5 percent had new cancers. That implies that around 5 percent of the people who haven’t returned may also have cancer, she says, but won’t know it. Similar scenarios are likely playing out at health systems across the country; a study that surveyed gastroenterology practices last year found that two thirds did not yet have a plan in place to follow up on missed appointments, although some have now begun this work in earnest.
Issaka is working diligently to contact and shepherd in her more skittish patients. One powerful tool is at-home detection tests for colon cancer. A low-cost fecal immunochemical test, or FIT, can detect blood or tumor DNA in stools and catch 70 percent of colon cancer cases [see “The Colon Cancer Conundrum”]. But a positive FIT result requires a follow-up colonoscopy, and scheduling that, Issaka says, remains challenging.
Telehealth has proved a surprisingly effective way to persuade overdue patients to visit the clinic. A study published in JAMA Oncology last spring examined the precipitous drop in breast, colon and prostate cancer screenings and found that telehealth patients were more likely to come in for exams. Patients who are concerned about in-person screenings can use telehealth appointments to talk with their primary care physicians about setting up a plan based on personal and familial risk factors, says the American Cancer Society’s Knudsen. “Screening is knowledge. It’s power,” she says.
Although much communication in oncology, particularly of bad news, is best done in person, the pandemic has shown that telemedicine can play an important role in cancer care and should remain in place, says Choueiri, who is also a professor of medicine at Harvard Medical School. “It’s helped a lot,” he says. “We can stay in touch with patients, maybe even better than before.”
The pandemic-imposed challenges to screening prompted the American Cancer Society to create tool kits explaining current screening guidelines in clear and simple language. It is also spreading the word that patient access to screening must be made easier. One way is to move screenings out of hospitals and into clinics and, when possible, even mobile vans. Another is to open up scheduling in off-hours. “Can you do screenings on Saturdays or in the evenings?” Knudsen asks. “Those turned out to be really popular times for mammography.”
Uncertain Mortality Models
There is little doubt that the chaos ushered in by the pandemic will lead to more cancer deaths. But determining how many has been difficult: many cancers are slow-growing, their development can be complex, and factors such as treatment decisions play a big role in outcomes. To assess how missed screenings might affect cancer mortality rates, the National Cancer Institute turned to Oguzhan Alagoz, a professor of industrial and systems engineering at the University of Wisconsin–Madison whose research involves modeling both cancer epidemiology and infectious diseases.
“The question is really interesting because it’s a combination of the two areas I work in,” Alagoz says. His first estimates, unveiled in a widely read editorial published in Science in June by NCI director Normal E. Sharpless, showed that missed screenings might result in 5,000 additional deaths in breast cancer alone over the next decade. A separate group, looking at missed colon cancer screenings, predicted another 5,000 deaths.
When Alagoz produced his breast cancer estimates early in the pandemic, he thought the numbers might not be truly representative. So he worked to refine them, using better data with three powerful cancer models that incorporated numerous factors related to breast cancer—such as delayed screening, treatment effectiveness and long-term survival rates—and the nuanced ways they intersect to affect mortality over time. “Everyone can tell you what will happen immediately, but it’s hard to say what’s going to happen in five or 10 years,” Alagoz says. “If there’s a huge increase in smoking, you’re not going to see more lung cancer right away. You’re going to see that 10 or 15 years down the road.”
After a more detailed analysis and after seeing screenings rebound from what he calls the “panic phase” of March and April 2020, Alagoz now says those early mortality numbers were far too high. In revised estimates, published in the Journal of the National Cancer Estimate last April, Alagoz and his colleagues suggested the pandemic could lead to 2,500 excess breast cancer deaths in the coming decade, half as many as they had first predicted. “The entire estimate was too pessimistic,” he says. “Any individual death is sad, but if there is any silver lining, it’s that this isn’t as bad as we feared.”
One reason death rates may be curbed, Choueiri says, is that oncologists did aggressive triage work to screen and treat patients who needed care most. His hospital system reported fewer missed cancer diagnoses than he expected, and he thinks this was because people at highest risk of cancer and those with palpable symptoms were most likely to be screened even during the pandemic’s most dangerous peaks. “Screenings never stopped 100 percent,” Choueiri says. “Who were the patients who continued to be screened? They were the highest, highest risk.”
Some oncologists say this “risk stratification”—prioritizing screening, diagnosis and treatment for those most at risk or with obvious symptoms—should stay in place after the pandemic ends so treatment can be provided quickly to those who need it most.
COVID’s Long Shadow
Understanding the pandemic’s effects on cancer mortality is a complicated task because delayed screenings aren’t the only factor involved. Increased alcohol consumption and reduced physical activity—behaviors common during long pandemic lockdowns—can increase cancer risk as well. But postponing an exam can be a major danger. In November 2020 Vincent Valenti, a retired screenwriter in Brooklyn, noticed his voice was hoarse. He attributed it to all the screaming he did on election night. But it persisted for weeks, and his girlfriend encouraged him to get it checked. Valenti, 71, refused. He wasn’t going near a hospital or doctor until he was vaccinated. “You walked by hospitals, and there were all these morgue trucks parked outside,” he says. “I knew something was wrong, but I wasn’t going to go near a hospital.” In February of this year, once he had received two doses of vaccine, he scheduled an appointment with an E.N.T. “She scoped me and jumped back,” he says.
There was a tumor on his larynx, stage 3, that had almost reached his lymph nodes. It was a shock to both Valenti and his doctor. He wasn’t considered high risk for laryngeal cancer because he doesn’t drink heavily or smoke. After seven weeks of chemotherapy and radiation, Valenti says, there was no trace of the tumor, and a recent PET scan confirmed that the cancer did not metastasize. Valenti was told his cancer would likely have been caught at stage 2, or even stage 1, if he had gone in right away.
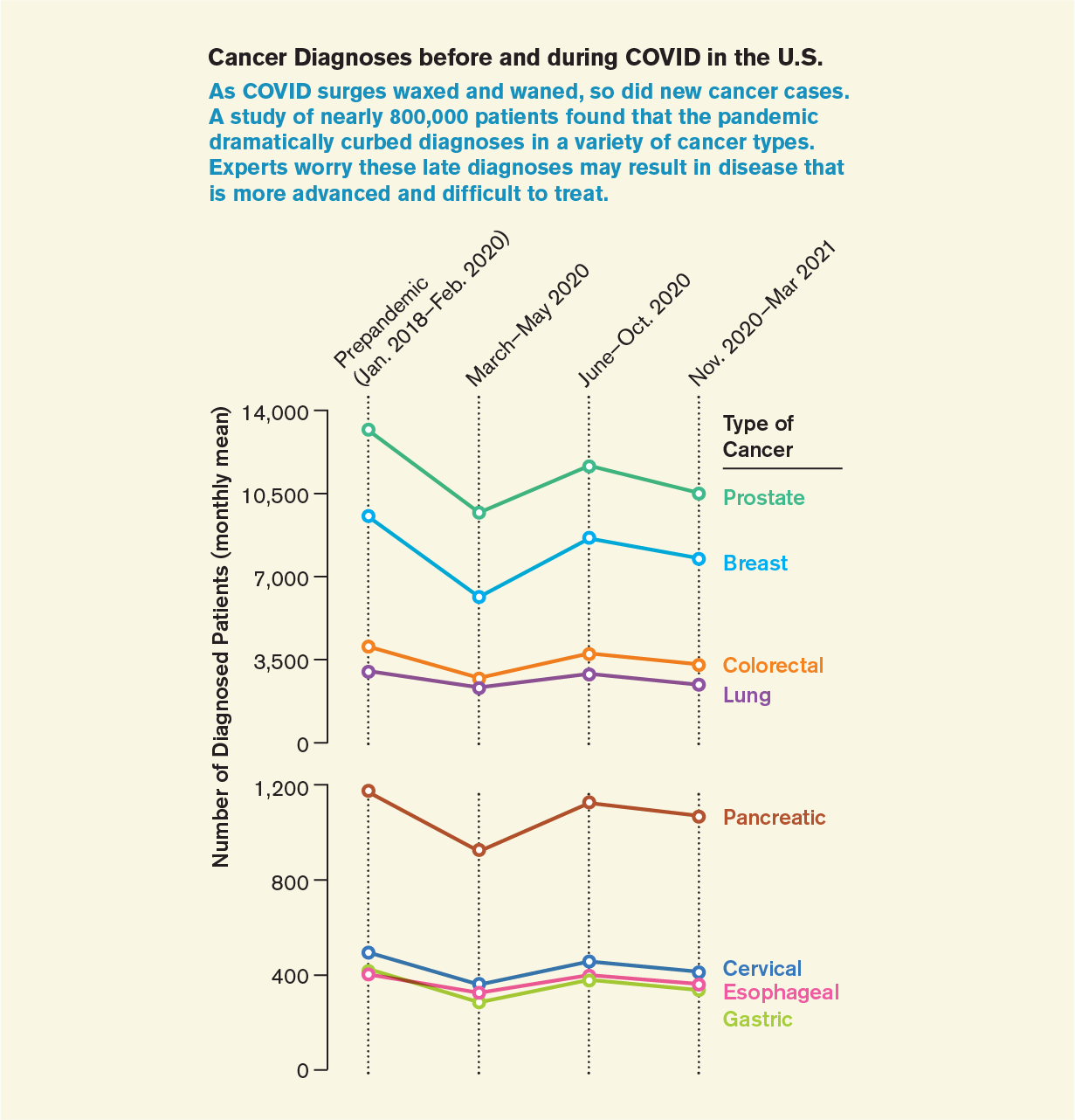
Research published in JAMA Network Open in August shows that Valenti is far from alone. The study reports that diagnoses of eight cancer types dropped nearly 30 percent during the first pandemic wave of 2020, rebounded somewhat during the summer and early fall, then fell by 20 percent during the pandemic’s winter surges. Such consistently low numbers indicate that many cases will continue to be undiagnosed, the authors wrote.
Some programs have already reported an increase in the detection of cancers. Lung cancer, the nation’s leading cause of cancer death, is of particular concern because it can be so aggressive. The University of Cincinnati’s lung cancer screening program was closed for three months. When screening resumed, patients remained scarce, and no-shows were frequent. But among those who did come in, “we noticed we were seeing many more suspicious lung nodules than usual,” says Robert Van Haren, a thoracic surgeon and assistant professor of surgery at the University of Cincinnati Medical Center, who analyzed the effect of the pandemic on cancer screenings. “Even small changes in the size of a lung cancer can be important for overall survival,” he says. “That’s the reason we’re concerned about any delays or stoppages.”
Whether the pandemic has already caused an increase in dire cancer prognoses more broadly is still an open question. Choueiri hasn’t run the numbers and is not sure yet whether his practice is facing more advanced cancer diagnoses. So far the picture is worrisome to him, but it is less so than he originally feared.
This is largely because screening did rebound. If the pandemic was turning out to be a natural experiment on the toll of missed cancer screenings, thankfully it was one that ended earlier than expected. “Testing for many cancers, such as mammograms, has largely returned,” says Choueiri, who has co-authored several studies tracking the pandemic’s effect on cancer screening. “Why did it return to normal? Simply because the hospitals, and all of us, put measures into place to make this as safe as possible.”
Deepening Health Disparities
But timely screening hasn’t returned for everyone. Those looking at the data see disturbing gaps in the populations that are coming back and those that aren’t, gaps that may be deepening racial and ethnic disparities in cancer care and mortality. At his health system, Choueiri says, fewer Black and Hispanic patients rescheduled mammograms from June to December 2020, even after screenings rebounded in other groups. Van Haren saw something similar in his Cincinnati clinics: more screening no-shows for patients at highest risk of lung cancer death, including those who were current smokers and those who were Black. “It’s concerning,” Choueiri says. “The pandemic may have accentuated racial disparities related to cancer screening that already existed.”
Black people are already 40 percent more likely to die from colon cancer than other groups. Issaka fears those numbers could now grow worse. “Before the pandemic, African-Americans, Hispanics and Native Americans were not screening at high rates. With COVID, my concern was that these same populations that were hard hit by the pandemic wouldn’t come for screening,” she says. “I worry that five to 10 years from now, we’re going to see patients in those groups presenting with advanced disease and higher mortality.”
Because colon cancers are usually slow-growing, it’s not too late to prevent these deaths. “We need to be very proactive,” Issaka says. “We still have the opportunity to turn the tide.”
One of the people working to do so is Kathy Briant, assistant director for the Fred Hutchinson Cancer Research Center’s office of community outreach and engagement. Cancer-screening outreach was one of the pandemic’s biggest casualties, particularly among racial, ethnic and low-income groups that have historically had lower access to screening tests and are far less likely to be up-to-date on cancer screening than white and high-income patients.
Briant has had to mothball the giant inflatable walk-through colon she used to send to events in tribal areas and gatherings of agricultural workers throughout Washington State. She has had to cancel all face-to-face meetings with at-risk older people, the same ones who are less likely to see her team’s YouTube and Twitter messages. Hardest of all, she says, she had had to call off two years of health fairs that, prepandemic, provided information, cancer screenings, free health tests and colonoscopy scheduling.
The communities Briant works with are both the least likely to receive cancer screening and the hardest hit by -COVID: minorities, frontline workers, and people who were losing jobs, struggling financially and dealing with SARS-CoV-2 infections. She learned relatively quickly that cancer screening was not a priority for many in these communities. There was fear of -COVID, but there were other reasons, too: no time, no child care, a lack of health insurance or the inability to afford copays. In addition, their regular clinics often were too overwhelmed with COVID patients to provide wellness checks or screenings.
People had more immediate needs, such as finding transportation to vaccine appointments and someone to help if they had COVID. Briant’s team pivoted from providing grants for cancer screening to helping in other ways. “Our agenda, yes, is cancer screenings, but we had to set that aside and listen to the community,” she says. “They were thinking about survival. They were saying cancer screening is not important right now.”
Issaka’s research confirms what Briant was seeing. One study at her safety-net hospital found that patients already faced multiple obstacles to having a colonoscopy, including lack of transportation, no coordination among specialists to get tests scheduled, and difficulties with the bowel preparation needed for the test. The pandemic added more barriers, she says, such as requiring a negative COVID test before people could even walk through the door.
By responding to more immediate needs, Briant’s team hoped to strengthen bonds and increase trust in communities they work with, something that will help them spread the cancer-screening message in the future. Sure enough, as restrictions loosened, she began fielding calls from community health leaders who wanted the inflatable colon sent over. The hypercontagious Delta variant has put those plans on hold—a colon is an enclosed space after all—so they have resorted to a video version until Briant can once again unleash her colon into the world.
Could We Be Overscreening?
Another piece of the cancer puzzle that the pandemic experiment may start to solve is a particularly contentious one. As cancer-screening programs continue to grow, an increasingly vocal group of physicians is arguing that too much screening might, at least for some people, be doing more harm than good.
These researchers contend that many patients, particularly those of advanced age, often receive more screening than they require. And those tests can result in more risk than benefit. “One of the biggest risks of cancer screening is the overdiagnosis of cancer tumors that are indolent and will never cause symptoms,” says Jennifer Moss, an assistant professor in the department of family and community medicine at Pennsylvania State University, whose research has shown that 45 to 75 percent of older adults receive screening they do not need. She found that for colon, cervical and breast cancers a large percentage of patients were being screened after they had aged out of the recommended age limit. In all three cancers, overscreening was more common for people living in cities compared with those in rural areas.
Unnecessary screenings not only result in false positives but also come with other issues, including unnecessary medical procedures to remove cancers that might not cause harm and side effects, such as perforations during colonoscopies. Now they have the added threat of SARS-CoV-2 exposure. “Many older patients face greater risk from cancer screening than not screening,” Moss says. “Especially in a time of COVID.”
Moss wants to be clear that people who need screening, based on national guidelines and conversations with their physicians, should get it. And she believes that the pandemic will likely cause an increase in cancer deaths because of missed screenings. But she also thinks the past year and a half will yield important data on missed screenings that were not as consequential, data that could inform future guidelines. “The pandemic will definitely give us insight into when, and how often, and for whom, cancer screening is the most effective,” she says.
Choueiri, for his part, is convinced that cancer screening is a singularly powerful tool that can catch cancers at their earliest and most treatable stages. “You don’t want stage 1 to become stage 4,” he says. “Or even stage 2.”
These days his conviction is personal. Unlike many of his patients, who postponed their screenings during the pandemic, Choueiri did not. Because of the pandemic slowdowns, he had extra time on his hands. So, when he turned 45 last year, he took his doctor’s advice and scheduled a routine colonoscopy. He didn’t think it was urgent—he had no symptoms or family history of the disease. But his test turned up an unexpected precancerous polyp. Now, he says, he will not miss any future screenings.
This article is part of “Innovations In: Cancer Early Detection,” an editorially independent special report that was produced with financial support from Johnson & Johnson.