When bacteria make their way into wounds, they literally threaten life and limb—unless they are detected as quickly as possible. Now a new sensor can nestle in bandages and alert a nearby smartphone when the bacterial population tips over into dangerous territory.
Healthy human skin is covered with bacteria that are quick to colonize an open wound, such as Staphylococcus aureus and Escherichia coli. To prevent these organisms from spreading through the body, which can permanently injure or kill a person, the infected wound may need to be cleaned and treated with antibiotics or—in the most extreme situations—an affected limb may require amputation. Medical professionals typically identify infections by unwrapping and observing a wound or by swabbing it and conducting a laboratory test. But removing a wound’s dressing can slow down the healing process. Plus, observations are subjective, swab tests take time, and both require that a patient be physically present.
To address these issues, some research teams are developing devices that sit under bandages and continuously monitor indirect signs of infection, such as changes in wound temperature or acidity. And scientists at the National University of Singapore have now created an even more direct infection sensor.
This sensor can detect an enzyme called deoxyribonuclease, or DNase. The enzyme acts as a reliable infection indicator because disease-causing bacteria produce it in large amounts inside wounds, whereas bacteria on healthy skin do not—so testing for the substance reduces the chance of a false positive result. Furthermore, DNase builds up before other infection signs appear. The new alert system (dubbed the “wireless infection detection on wounds,” or WINDOW, sensor) was detailed in Science Advances.
WINDOW’s enzyme-sensing parts rely on a gooey material called DNA hydrogel, or DNAgel, made of entangled chains of DNA. The researchers developed a particular kind of DNAgel that remains stable in watery environments, such as the human body, but begins to break down in the presence of DNase. They connected this gel to a chip that senses when the gel decays and responds by sending a signal to a smartphone. This signal is broadcast using a battery-free wireless process called near-field communication, the same technology that allows people to make a payment with the tap of a credit card.
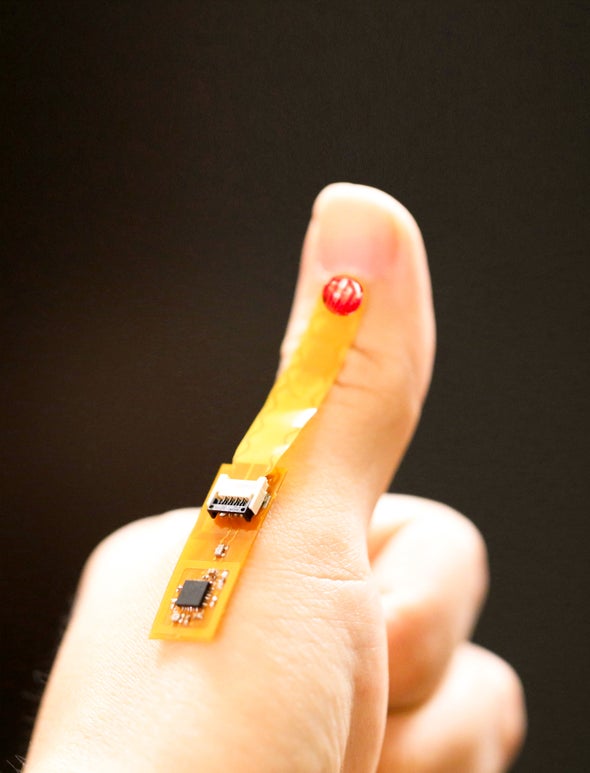
“By coupling this DNAgel with that sensor [chip], we can make a completely battery-free device that can fit under a bandage on the wound,” says study co-author John Ho, an electrical engineer at the National University of Singapore. A person with a chronic wound or someone sent home after a surgical operation might monitor their own status by tapping a smartphone next to their dressing a couple of times a day. If the phone receives an infection alert, it can send a message to a doctor or tell the patient to return to the hospital for an antibiotic treatment.
Other researchers have tried different approaches to infection detection, including high-tech imaging to monitor bacterial spread and “electronic noses” to sniff out an infection’s chemical signals. “There’s a raft of stuff out there that people, in principle, have proved” works, says June Mercer-Chalmers, a project manager at the University of Bath in England, who was not involved with the new study but worked on a team that developed a low-cost ultrafast swab test for infections. The issue, Mercer-Chalmers says, comes down to a tool’s practicality: whether it requires a lot of cumbersome equipment, if it has steep barriers to legal approval, and how cost-effective it is. She points out that the WINDOW sensor requires electronic parts and smartphone access, which might put it out of reach for some people and hospitals systems. Ho says the material cost of each WINDOW sensor is under $10, noting that it could be constructed with existing electronic manufacturing methods.
Thus far Ho’s team has exposed the DNAgel to wound swabs from 18 people’s diabetic foot ulcers, some with S. aureus infections, to see how much the material degraded in the presence of the bacteria. The researchers also used the device on six living lab mice whose wounds were exposed to the same bacterial species, and it successfully detected infections within 24 hours—before any physical signs had become visible. Because the WINDOW sensor is still in its early days, Ho plans to continue testing it on larger groups of patients and on wounds infected with other kinds of bacteria. “Hypothetically, this should work with many other types of strains as well [because they] have similar DNase-secreting mechanisms,” he says.