Masks and testing have been key to the COVID-19 pandemic response—and now devices that combine the two may be on the way. Harvard University and Massachusetts Institute of Technology researchers used synthetic biology to create a face mask that accurately detects the COVID-causing virus.
Synthetic biologists use biological parts to build various devices, including sensors that detect genetic sequences. Previous efforts have used engineered bacteria in these sensors, but living cells bring challenges (like keeping them fed) and biohazard risks. The new research makes wearable devices with freeze-dried “cell-free” circuits built from genes, enzymes and other cell components, which can be placed on porous, flexible materials and easily stored. (The researchers described adding such circuits to paper in 2014.) “This work's important advance is converting bench-top technology to wearable devices,” says bioengineer Xinyue Liu, who develops living sensors at M.I.T. and was not part of the new study. Such tools could allow for simplified on-site testing.
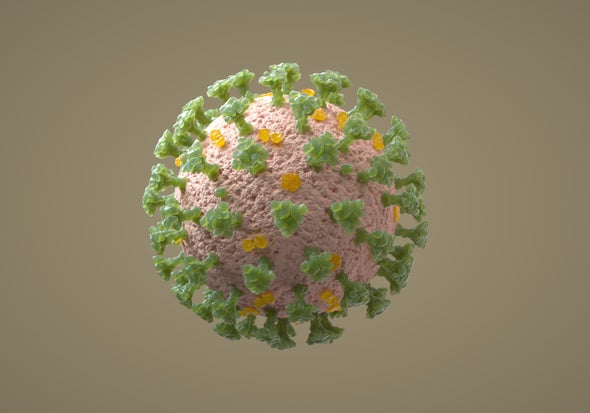
The study, published in Nature Biotechnology, describes adding cell-free sensors to elastics, textile threads and paper to detect the virus that causes COVID-19 (SARS-CoV-2), Ebola virus, MRSA, a chemical nerve agent and more. Some of these sensors, including those used in the new face mask that flags SARS-CoV-2, rely on CRISPR technology: When “guide” RNAs match target DNA, they activate an enzyme that cuts the nucleic acids (the DNA “letters”). This particular enzyme also cuts other nearby nucleic acids, freeing a fluorescent protein that emits light. The technique makes for versatile, “programmable” sensors that could be quickly adapted to detect virus variants.
The prototype mask activates with a push-button that rehydrates the sensor, starting reactions that break the virus apart and amplify its DNA for detection. The full process produces a color change within 90 minutes of activation—say, when worn by a hospital patient. “Breath is a nice source of noninvasive sampling that has the right concentrations,” says University of Freiburg sensor expert Can Dincer, who was not involved in the new study. “The application really fits the needs of our current situation.”
Sensitivity was similar to most lab tests'. “The ‘gold standard’ would still be your lab-based PCR tests, but we're in the ballpark,” says bioengineer and senior author James Collins. The single-use masks need no power source nor operator expertise and work at typical room temperature and humidity.
Collins hopes to commercialize the mask to sell for around $5. Similar genetic-circuit wearables, he adds, could aid health-care workers, military personnel, first responders, and others in the field.