If you were paying attention to social media recently, you might have come across a viral ad for EXTRA gum depicting scenes of postpandemic life: people slowly peeking out from behind closed doors, shutting their laptops before bursting maskless out of their toilet paper–filled dens into the street. The actors, all unwashed and unkempt, run gleefully to the nearest park where each proceeds to pounce on the first stranger they encounter and initiate a passionate make-out session, set to Celine Dion’s power ballad “It’s All Coming Back to Me Now.”
It’s been over 100 years since the “Spanish” flu pandemic stifled our sex lives to the extent that we’ve experienced during COVID-19. As a sexual health physician and researcher, I can attest to seeing empty waiting rooms for months as people kept their social and sexual distance, their desire squelched by fear of contagion. Certainly there were some for whom pandemic-induced abstinence was short-lived, and I was gratified to see public health agencies in New York and Canada cheerfully providing guidance on the matter: encouraging masked sex or even use of glory holes in barriers such as bathroom doors to facilitate anonymous oral sex.
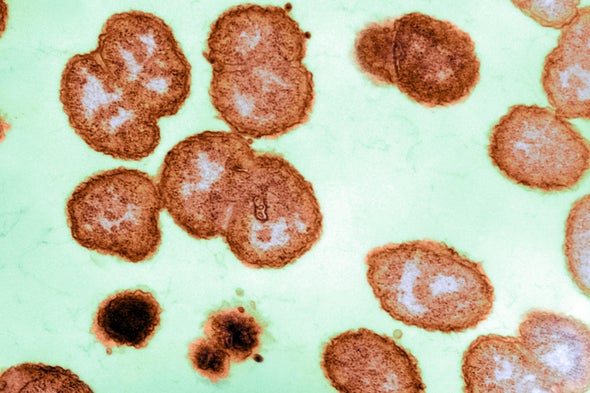
For the most part though, our sexual appetites languished alongside our psyches as we exhausted our energy just trying to survive. And it wasn’t just Americans: studies from the U.K., China, Israel and Australia found that 40–60 percent of people reduced their number of sexual partners or the frequency of sex during the pandemic. As a consequence of our collective abstinence (plus a national shortage of testing kits), rates of sexually transmitted infections (STIs) in the U.S. plummeted in the second quarter of 2020, after previously reaching record highs in 2019.
Now that vaccines have arrived in the U.S. en masse, there’s little holding us back from having sex again. Celine Dion’s ballad would imply that our muscle memory around sex will be like that of riding a bicycle: even if we haven’t done it for a while, we still haven’t forgotten how. What isn’t clear is whether we’ll still have the drive. For nearly two decades prior to the pandemic, American sexuality had been on a downward slope, even among the most sexually active age demographic. In a study of over 9,000 adults based on surveys from 2000 to 2018, a third of young men aged 18–24 reported no sexual activity in 2018; activity also declined over the study period for both men and women aged 25–34.
For those of us who do resume having sex, it's logical to think that a year of living with COVID, donning masks, getting tested and negotiating safe socializing would translate to discussing safer sex. Not so, says Lisa Wade of Tulane University, who has interviewed over 120 college students about sexual behavior during the pandemic. Despite a diversity of race, sexual orientation and prior sexual experience among her study participants, when asked whether living through COVID has changed the way they think about sex and STIs, their responses are “strikingly consistent”: a wrinkled nose, a look of confusion, and a resounding “no.”
Wade’s students are testing 2–3 times per week for COVID and have no qualms about asking each other about their test results. Yet asking about testing for STIs does not come as naturally. STIs are still accompanied by a stigma that shrouds these discussions in judgment along the lines of, “Why would you need to test?” and “What have you been up to?” Even those who felt comfortable asking others to wear a mask can find it awkward to ask a partner to use condoms or are met with resistance when such requests are made.
Our resistance to condoms and barriers cuts across gender, age and sexual orientation. HIV researchers have long understood the concept of “condom fatigue” among men who have sex with men, a weariness experienced after years being told to use condoms by HIV prevention campaigns. As Benjamin Klassen of Simon Fraser University found in 2019, condoms among gay men now hold similar status as public transportation: something you’d love everyone else to use without having to use it yourself.
Condoms are losing popularity with the Generation Z set as well, even though teens are the age group most likely to use condoms. According to the CDC’s Youth Risk Behavior Survey, condom use by high school students during their most recent sexual encounter declined from 62 percent in 2007 to 54 percent in 2019. The outlook is even worse for dental dams, squares of latex placed over the vulva for oral sex. Juliet Richters of University of New South Wales found less than 10 percent of Australian women who had sex with women had ever used a dental dam, and only 2 percent used them consistently.
In our current era of technological innovation, it seems like we should have something better than barriers—perhaps a smartphone app or an STI-blasting laser. Yet condoms remain the only multipurpose prevention device that provides both contraception and protection against STIs/HIV. But hopefully that’s set to change. Groups such as the global Initiative for Multipurpose Prevention Technologies (IMPT) are working to advance the development of at least 20 products: pills, rings, diaphragms, gels, injectables and implants, with each product providing protection against at least two conditions: unplanned pregnancy, STIs, or HIV.
What about building a better condom? The Gates Foundation tried to give it a go, offering $100,000 seed grants to companies in 2013 to develop a next-generation condom that “preserves or enhances pleasure” in order to “improve uptake and regular use.” By 2019 three of the 11 initial awardees had received an additional $1 million to advance to the clinical trial stage. Whether these products survived the pandemic and will make it to market remains to be seen. At least for the moment, traditional condom sales are surging, but unlikely to endure long term as we fall back into our old usage patterns.
Then there’s always hope of an STI vaccine. While there are none immediately forthcoming, new clinical trials are ongoing for vaccines against herpes and gonorrhea. And as Operation Warp Speed has shown, pharmaceutical companies can create effective vaccines quickly with enough political will and financial support.
But whether the future of prevention is a better condom, a new device or an STI vaccine is unimportant. What’s crucial is having prevention products that people will actually use. If predictions of a Roaring Twenties redux or a post-COVID Summer of Love hold true, then a rise in STIs and HIV are sure to follow. It will take more than our old barrier methods to meet the current needs of our sexually diverse population. We must invest in development of new prevention products now, or risk being caught with our pants down later.
This is an opinion and analysis article.