COVID-19 triggers a strong immune response in most people. Yet several recent studies observed that the amounts of antibodies in those recovering from the virus appear to decline within a few months of infection. The findings set off a frenzy of speculation that immunity to the virus may not last long, throwing cold water on hopes for a vaccine. Many scientists say such worries are overblown, however.
A June 18 Nature Medicine study conducted with a small group of patients in China showed that in both asymptomatic and symptomatic individuals with COVID-19, antibody levels dropped significantly during recovery—and that the levels became undetectable in 40 percent of the asymptomatic group. A preprint study by researchers in England that was posted online in mid-July similarly demonstrated that antibody levels declined substantially within a few months of infection and that people with less severe illness had fewer antibodies. And most recently, a small study, published on July 21 in the New England Journal of Medicine, found a “rapid decay” in antibodies among individuals with mild cases of COVID-19.
These results may sound universally grim. But several experts Scientific American spoke with said they thought that the declines were not as scary as initially portrayed, that some reduction in antibodies is normal and expected and that antibodies are just one piece of the immunity puzzle. Evidence from other viruses and animal studies of SARS-CoV-2 infection provide reason for optimism, they add. That assessment is no doubt reassuring for vaccine developers, some of whom are already racing ahead with large-scale clinical trials. Only longer follow-up studies of people infected with the novel coronavirus will show whether antibodies confer lasting protection, however.
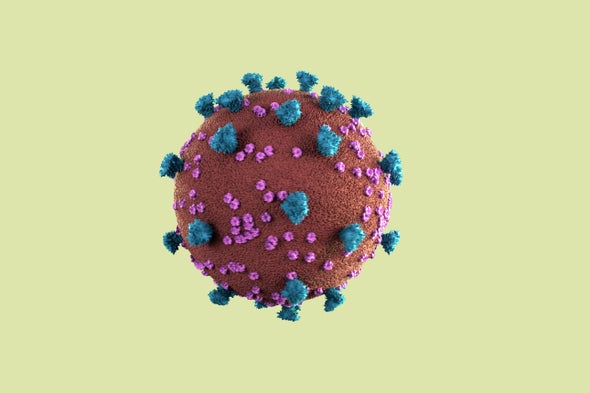
The human immune system consists of two parts: The innate immune system mounts a nonspecific response to invaders that occurs within hours of infection. In contrast, the adaptive immune system launches a targeted reaction to a particular pathogen, which can take weeks or months to develop. The latter system consists of three parts: antibodies, B cells and T cells. Together they recognize and fight off the invader and can store a memory of it in case of future infection (vaccines similarly work by creating a fake “memory”). Some of the antibodies, known as neutralizing antibodies, can bind to a specific part of a pathogen and deactivate it. Scientists hypothesize that these antibodies’ presence in people who have had COVID-19 may be one key signal of immunity.
The recent studies documenting patients’ antibody decline have triggered some scary headlines proclaiming that any immunity to COVID-19 may be short-lived. In the NEJM study, Otto Yang, a professor of medicine and associate chief of infectious diseases at the David Geffen School of Medicine at the University of California, Los Angeles, and his colleagues measured antibodies in 34 people, the large majority of whom had clinically mild coronavirus infections, at an average of 37 and 86 days after symptoms appeared. “What we saw was that the amount of antibodies against the virus dropped very dramatically in that time period”—by about half every 36 days, he says. (The paper originally described a half-life of 73 days, but this figure was found to be a mathematical error.) Yang adds a few caveats: Scientists do not know if antibodies are protective against SARS-CoV-2 infection—although that possibility is a reasonable guess—or how much protection they might confer. And they are not certain they are measuring the right type of antibodies. Nevertheless, he says, “the decline that we see is strikingly fast.”
Other scientists interpret the decline as less worrisome and in line with that observed in other viruses. In reference to the NEJM study, Florian Krammer, a professor of microbiology at the Icahn School of Medicine at Mount Sinai, tweeted, “I fail to see the rapid decay here.” Using a test developed by Krammer and his team, a preprint study led by his colleague Ania Wajnberg found a much more modest decrease in antibodies. In some cases, people who had fewer antibodies at first even showed a small increase over time.
Seeing a slight reduction in antibodies is fairly normal, says Wajnberg, an associate professor at the Icahn School of Medicine. “Frankly, that’s not that surprising, because you’re not sick anymore,” she says. Once a person has successfully fought off the infection, you would expect his or her antibodies to approach a lower, baseline level. If that individual was reinfected, the B cells could then ramp up the number of antibodies again, Wajnberg says. Or maybe that baseline level itself would prove enough to be protective. “What we don’t want to see is: two weeks later, [antibodies] go to zero. Honestly, that would be very unexpected,” Wajnberg adds. But the fact that antibodies wane over time is not shocking, she says.
Viral immunologist Zania Stamataki agrees. “The data on the decline of the antibodies is not scary. We’re seeing a tiny drop, which is quite expected,” says Stamataki, a senior lecturer at the University of Birmingham’s Institute of Immunology and Immunotherapy in England. “I don’t think there is this really rapid decay like people have reported.”
Yang stands by his interpretation of a steep decline, saying it agrees well with the Nature Medicine study and English preprint paper. He says the reason for disagreement may reflect the populations being studied. Yang and his colleagues looked at people with clinically mild infections who had lower initial levels of antibodies, whereas those who have higher levels to start with “may actually also have more persistent antibodies,” he says.
Stamataki and others caution that it remains to be seen whether any level of antibodies can shield against reinfection. “The fact that we can pick up antibodies in patients that have been infected with coronavirus does not mean that they are protected,” she says. “It means that they can recognize the virus and make the right immune response that could potentially be protective in the future.” Researchers still do not know what amounts and types of antibodies will prevent reinfection six or seven months later, “but we will soon find out,” she adds.
Scientists have focused on antibodies because they are relatively easy to measure with a blood test and may be helpful as a treatment for COVID-19. But the adaptive immune system also involves T cells, which may mount a strong response to the novel coronavirus even if antibodies have waned. In May Alessandro Sette and Shane Crotty, both at the La Jolla Institute for Immunology, published a study showing that SARS-CoV-2 produces a strong T cell response, particularly to the virus’s “spike” protein, which it uses to gain entry to cells. And a preprint study by researchers at the Karolinska Institute in Sweden found such responses in people with mild or asymptomatic COVID-19, including when antibodies were undetectable. So even without antibodies, T cells could keep a record of the infection. But its strength may depend on that infection’s severity. “The memory is proportional to the perturbation to the insult—how much of a scare the immune system has,” Sette says. “If it's a very mild infection, it might not create enough of an immune response, in the first place, to create a long-lasting memory.” In fact, Stamataki says, it is possible that some people may clear SARS-CoV-2 using the innate immune system—without developing any memory of it. If they then encountered the virus again, they could potentially get COVID-19 a second time.
There have been a number of anecdotal reports of people getting reinfected with the novel coronavirus, but no substantive proof has been established. There are other explanations: people with weak immune systems might not be clearing the virus totally, or tests might be picking up remnants of it that are not infectious, Stamataki says. While true reinfection is not impossible, it would likely occur in only a small minority of people, she adds.
Scientists still do not know what level of immune response might be protective against future infection. Only longer-term studies will be able to answer that question. Wajnberg says her colleague Viviana Simon, a professor of microbiology at the Icahn School of Medicine at Mount Sinai, is currently leading a study to monitor a few hundred health care workers, with and without antibodies, over the course of a year or two to see who gets COVID-19 and who does not. Yang says he and his team plan to continue monitoring more than 60 people for a year as well.
In the short-term, though, animal research offers some clues. One study found that monkeys that were previously infected with the novel coronavirus and developed antibodies did not get sick when they were later reexposed. But monkeys are not humans, of course. And deliberately exposing people to the virus raises clear ethical issues, so we will likely have to wait for more data to accumulate over the next few months. “We need to be patient,” Sette says.
Read more about the coronavirus outbreak from Scientific American here. And read coverage from our international network of magazines here.