My first day in Mexico City was tough. The smog was so thick that I gasped for breath while climbing the stairs to my hotel room. I had braced for headaches from the high altitude and thin air, but I was not prepared for how dirty that air was or for the bloodshot eyes and burning lungs.
Declared the world's most polluted metropolis by the United Nations in 1992, greater Mexico City has worked hard to clean up its act. To some degree it has: the city is rightfully proud of its miles of bike paths and lush parks. Yet a casual glance at the smudged horizon shows that those efforts are not enough. Most days the area has levels of airborne sooty particles that greatly exceed standards set by the World Health Organization, as well as elevated amounts of other pollutants. Clogged with more than 9.6 million vehicles and an estimated 50,000 smokestacks, Mexico City stews in a toxic brew known to corrode human lungs and hearts. Now many scientists agree that this pollution also damages the brain.
In 2018 a study found lesions known to be hallmarks of Alzheimer's disease in the brains of Mexico City residents in their 30s and 40s—decades before signs of the disease normally can be detected—and tied this damage to exposure to the city's bad air. The researchers who did that work, who are from institutions in Mexico and the U.S., have also found early forms of this frightening damage in infants and young children. And Mexico City is not the only place where bad air has been linked to Alzheimer's. Just a few years ago a team of Harvard scientists released data from a large study of 10 million Medicare recipients ages 65 and older living in 50 different cities in the northeastern U.S. The researchers reported a strong correlation between exposure to specific air pollutants and a number of neurodegenerative disorders, including Alzheimer's.
Other studies in England, Taiwan and Sweden—among other countries—have turned up similar results. “Air pollution is emerging as one of the hottest areas in Alzheimer's research,” says George Perry, a neurobiologist at the University of Texas at San Antonio and editor in chief of the Journal of Alzheimer's Disease. In a field where scientists have spent decades focused on genetics and the buildup of damaged protein fragments called beta-amyloid as causes of the disease, Perry says, now many experts agree that air pollution plays a major role. This assessment is echoed by Masashi Kitazawa, a toxicologist at the University of California, Irvine, and an expert on environmental toxins. “Genetics is huge in Alzheimer's research, and for years almost no one wanted to look beyond genes,” he says. “But in the past three or four years the number of papers linking air pollution and cognitive decline has exploded.” For the most common form of Alzheimer's, known as late-onset disease, researchers now estimate that at least 40 and as much as 65 percent of the risk involves nongenetic influences such as lifestyle and harmful environmental exposure. Air pollution is one of the leading factors.
Much of this concern centers on airborne toxin-packed droplets or solid bits that are about one 30th the diameter of a human hair. Known as fine particulate matter (called PM 2.5 for its specific size), it typically comes from burning oil and gas in cars and trucks and power plants, as well as from burning coal or wood. These particles are inhaled deep into the lungs and can pass quickly into the bloodstream. Scientists have demonstrated that when PM 2.5 enters the body this way, it wreaks havoc on human respiratory and cardiovascular systems, leading to cancer, heart attacks, strokes and early deaths.
Scientists once thought that the brain was protected from similar carnage by the blood-brain barrier, a network of closely packed cells lining blood vessels of the brain that prevents toxic substances from passing from the blood into brain tissue. Unfortunately, there is now compelling evidence that PM 2.5 can and does enter the brain via two pathways. First, the particles can alter the blood-brain barrier itself to make it more permeable to pollutants. Second, the particles can bypass the barrier altogether by slipping from the nose into the olfactory nerves and then traveling to a part of the brain called the olfactory bulb. The brain, it turns out, is no more protected from the relentless assault of air pollution than is any other organ.
High exposure
Much of the recent work linking poor air quality and brain disease has its roots in the early research of Lilian Caldern-Garcidueas, a physician and neuropathologist at the University of Montana. Born and raised in a town not far from Mexico City, Caldern-Garcidueas has studied the health impacts of the region's foul air for decades. In the early 2000s she examined 40 dogs roaming the most polluted parts of Mexico City and found Alzheimer's-like pathology in their brains. This discovery prompted her to look at the brains of humans who had lived in similar neighborhoods. What she saw—Alzheimer's-associated proteins in the brains of children and infants as young as 11 months—alarmed her. “Exposure to air pollution,” she wrote in 2008, “should be considered a risk factor” for Alzheimer's, in particular for those who are genetically predisposed to the disease.
Caldern-Garcidueas's conclusions have been substantiated by other scientists. Jennifer Weuve, associate professor at the Boston University School of Public Health, led one of the first U.S.-wide investigations into the link between air pollution and brain disease and published the results in 2012. “We had two hints on the relationship between the aging brain and air pollution,” she says. “The first was the impact of air pollution on the cardiovascular system—heart attacks and strokes. The brain relies on blood circulation, so naturally this raised concern that the brain, too, was being affected. The second hint was subtler. Toxicologists did some well-controlled studies of animals exposed to air with high levels of suspended particles and found that these particles got into the brain. Some of those particles contained known neurotoxins, like manganese. And we knew that couldn't be good.”
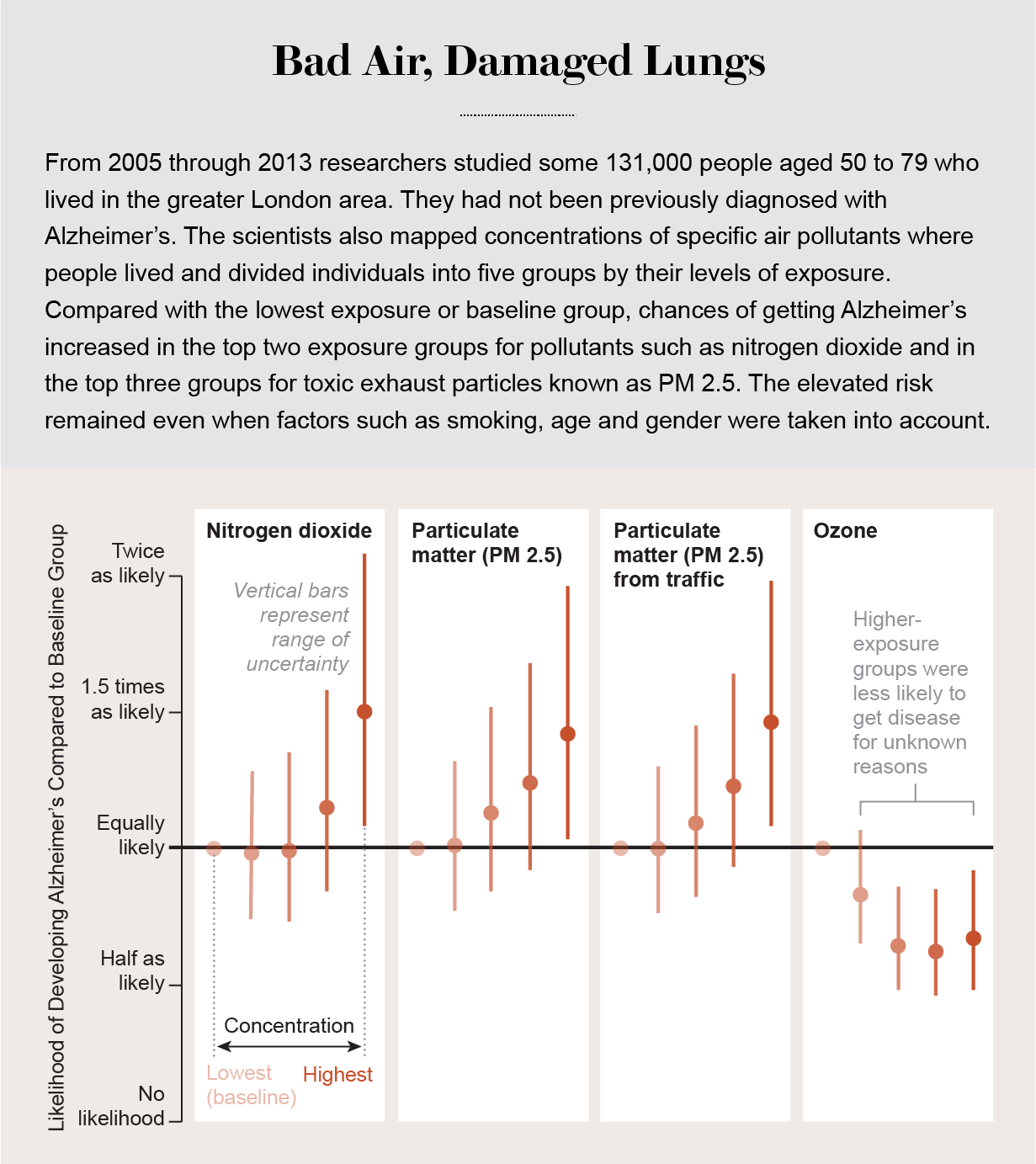
More epidemiological evidence of an airborne-particle problem has since piled up. In 2018 the BMJ published a study of some 131,000 London residents aged 50 to 79 and concluded that those with the most exposure to air pollution were the most likely to be diagnosed with dementia over the eight years they were observed. The link was particularly strong between Alzheimer's and PM 2.5 particles. A study of nearly 100,000 residents of Taiwan found similar results. Researchers in Sweden concluded that air pollution increased dementia incidence even among people with no genetic markers for the disease. And scientists at the University of Toronto looked at 6.6 million people in the Canadian province of Ontario and found that those who lived within 50 meters of a major road, where levels of fine pollutants are very high, were 12 percent more likely to develop dementia than individuals living more than 200 meters from those same roads.
From air to brain
Of course, epidemiological studies have limits. It is unethical to ask humans to knowingly expose themselves to polluted air over a period of months or years. This restriction makes it difficult to carry out controlled studies that eliminate many factors other than air pollution that might predispose residents of some regions to Alzheimer's and other forms of dementia.
“In a perfect world, everyone would wear an air-pollution monitor so that we could get real-time data on their exposures,” Weuve says. “But this is not a perfect world. So we work with experts to build estimation models. It's not enough. In the case of Alzheimer's, it's chronic, long-term exposure that counts, and we don't even have a worldwide registry of people with Alzheimer's, let alone the resources to follow people for many years prior to their acquiring the disease. So it is quite difficult to nail down causation.” Indeed, in some regions of the world, air pollution is so bad that people die of heart disease long before they would ever show symptoms of late-onset Alzheimer's.
To get a better handle on cause and effect, scientists have turned to animal models to search for biological mechanisms that may underlie a link between cognitive decline and various types and amounts of air pollution. In 2015 neurobiologist Colin Combs, chair of the department of biomedical sciences at the University of North Dakota School of Medicine and Health Sciences and an expert on neurodegenerative disease, pumped air containing different levels of particulate pollution into cages with genetically identical mice for different time periods. More exposure, he learned, produced more damage. “What we found supports the theory that long-term exposure to airborne particulate matter has the potential to alter the brain and promote the development of early Alzheimer's-like pathology,” he says. In 2018 scientists at Cedars-Sinai Medical Center in Los Angeles and their colleagues reported that heavy metals from polluted air not only found their way into the brains of rats after just a few months but also appeared to activate genes that trigger neurodegenerative disorders and cancer.
Air pollution might also interact directly with variants of certain genes associated with Alzheimer's, prompting the acceleration of brain aging and neurodegeneration in people who are already genetically susceptible. Not all people with late-onset Alzheimer's have these genetic markers, but many do, and the one-two punch of a gene-environment interaction seems to be particularly potent. Clinical psychologist Margaret Gatz of the University of Southern California explains that damage to the vascular system from pollution and other factors is associated with an increased risk of Alzheimer's and other forms of dementia, especially in people who have a genetic tendency to acquire the disease. “There's a good deal of evidence that vascular risk factors are more dangerous for carriers of the APOE4 variant of the APOE gene,” she says. “And for this and other reasons, a lot of research has focused on the genetic risk of the disease and all but overlooked the lifestyle and environmental component.”
What toxic substances found in air pollutants do when they get to the brain fits well with several ideas about the way Alzheimer's-related damage develops. Neurotoxicologist Deborah Cory-Slechta of the University of Rochester Medical Center says that in both animals and humans, these pollutants prompt the release of cytokines from microglia cells, the resident immune sentinels in the brain. Cytokines are signaling molecules that help to regulate immunity and inflammation. Under normal circumstances, this response can help protect the brain against outside invaders. But chronic exposure to polluted air can result in the overproduction of proinflammatory cytokines and chronic inflammation that leads to nerve cell death. “Ultrafine particles seem to be the most important factor in this process,” Cory-Slechta says.
She also notes that it is hard to zero in on specific components of these particles. “For one thing, we have very little historical data on them, so it's hard to judge their relative levels in the environment. For another, they contain lots of different substances that we tend to clump together,” making it difficult to know what specifically is causing the negative effect.
Particle pollution from the burning of fossil fuels and other sources contains hundreds of substances, ranging from noxious gases such as sulfur dioxide and nitrogen oxide to the dust emitted from automobile and truck brakes, tires and clutches. Cory-Slechta says that these pollutants tend to accumulate in the brain over many years, which might help explain why Alzheimer's is typically a disease of old age. But, she adds, there are still many unknowns about what exactly gets into the brain from the air—it's not clear that all these substances make it inside—and when those that do cause trouble. “What we do know is that iron, zinc, copper, and other metals are required by the brain, but at a specific level. What happens when that level is exceeded?” she asks. “We know that too much iron can lead to oxidative stress and neurodegeneration. We also know that some pollutants, like aluminum, play no essential role in the brain yet tend to accumulate there and provoke an inflammatory response. Frankly, I think we should be taking a closer look at that. And it's not just metals. Organic contaminants might also be involved in neurodegenerative disease.”
One type of such organic pollutants are lipopolysaccharides, large molecules released from bacteria spewed from waste-treatment plants and other sources. Scientists have found these molecules can latch onto particulates and, when inhaled, provoke an inflammatory response in the lungs. In animal studies, lipopolysaccharides and other organic matter have also been shown to provoke inflammation and related cognitive degeneration in the brain.
Particles and memory loss
Jiu-Chiuan Chen, a physician and epidemiologist at the University of Southern California, specializes in the study of airborne pollutants in the brain and says that although the impact of individual substances is still under debate, the overall effect of the mix is clearly related to brain damage and cognitive problems. Chen was co-author of a study published last year in the journal Brain that found clear links among fine-particle pollution, structural changes in the brain and memory loss in older women. Chen and his collaborators used neuroimaging and cognitive tests to measure brain changes and memory, plus a mathematical model that incorporated two sources of environmental air-quality data.
“What we found was that women with the highest exposure to pollutants showed an early decline in episodic memory,” he says. This type of long-term memory involves recalling a previous experience along with the time and place of the event and associated emotions. The decline Chen detected in these women appeared preclinically—before any actual symptoms of Alzheimer's—and was independent of the subjects' cardiovascular status. Alzheimer's research has established that people with a decline in episodic memory have a very high risk of developing the full-blown disease later in life.
“There are more than 10 studies that link late-life exposure to air pollution and dementia,” Chen says. “The evidence there is quite compelling. Whether exposure in early life is also a factor, we don't know. But in animal studies, toxicologists start exposure in early life, look at the pathological changes and see problems. It looks like small particles can accelerate the amyloid-deposit process, but we're not yet sure whether this happens in humans. And there might be a genetic component involved—that is, some people might be more susceptible than others to the effect of pollution. There might be a subgroup of individuals who are particularly susceptible and might be at greater risk. We don't yet have enough power in our studies to address this question, but I believe we will.”
Risk reduction
While the disease remains a horror facing millions of people around the globe, there is some encouraging news in these discoveries about air pollution, several scientists say: people can take action to diminish the hazards. Most drugs so far have not helped patients, says George Washington University epidemiologist Melinda Power, who focuses on identifying modifiable risk factors for cognitive decline and dementia. ”So at the moment, prevention through the reduction of environmental and lifestyle factors looks like our best bet,” she says. “And air-pollution exposure is looking [like it could be] very important.”
The evidence about brain damage is a strong argument for stricter air-quality controls, says University of Michigan epidemiologist Kelly Bakulski. “This is a really hopeful area,” he says. “Unlike our genes, environmental factors are things we can control—removing these pollutants from our communities will have no ill and many positive impacts.”
In addition, Gatz says that simple changes in how we live can help. “Physical exercise is shown to reduce risk,” she says, both because it increases blood flow to the brain and because it increases levels of brain-derived neurotrophic factor, a protein that promotes the growth and maintenance of brain cells.
Knowing the havoc that the disease inflicts, it is time to take such changes seriously. “We have the means to do it,” Bakulski says, “and given the risk of not doing it, we must.”