At 6 feet, 3 inches tall, Brett Muccino is a big man with a powerful frame, so he finds it hard to imagine how he could have flown through the narrow windshield of his old Ford Ranger. “It was a little, tiny thing,” he recalls. The devastating 1986 car crash crunched vertebrae in his neck and lower back. It also launched a 34-year battle with chronic pain and a love-hate relationship with the opioids he relied on to manage it.
On a sunny fall day Muccino was decked out in a hat and jacket emblazoned with the words “Vietnam Veteran” while visiting the West Haven VA Medical Center in Connecticut. He moved haltingly through the long corridors of polished linoleum, slightly bent over a walker. A bad back is not the only source of misery for this retired nursing home operations director. Diabetic nerve damage—the VA attributes his diabetes to wartime Agent Orange exposure—has rendered his feet and his hands painful, tingly and unreliable. He also suffers from chronic infections around an artificial knee.
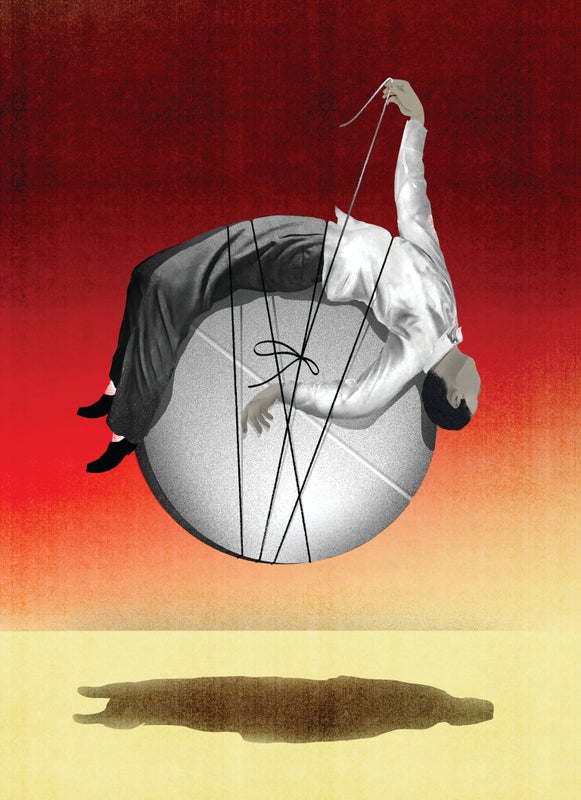
Muccino, now 68, had come to West Haven’s Opioid Reassessment Clinic after a long and perilous journey that included seven spinal surgeries and escalating doses of opioids when the operations, and physical therapy, failed to bring relief. In the 1990s doctors switched him from short-acting Percocet to 40 milligrams a day of a hot new drug: long-acting OxyContin. Within a few months he needed twice the dose, but “at least it allowed me to work,” he says. No one told him it was addictive. He found out when a surgeon cut him off shortly before a back procedure. “It was cold turkey with no discussion of what I was going to go through,” he recalls. Within 48 hours he was in an emergency room wracked by the agony of withdrawal—screaming in pain, shaking and unable to hold down food. Back on opioids, he began supplementing his prescription by buying drugs on the street and later from an unscrupulous doctor, taking upward of 320 milligrams of Oxy a day. He would try to get clean periodically, but pain always brought him back.
By the summer of 2016 Muccino was sick to death of the whole vicious cycle. After his final back surgery brought him some relief, he told his doctors, “I want off of everything.” His timing was good: a few years earlier the VA had opened this specialized clinic less than an hour from his home. Its team helped him learn a variety of pain-management techniques and gave him a medication that both reduces pain and controls withdrawal symptoms. Thus began a slow, many-months taper of Oxy that ended up at his goal: zero.

Muccino’s struggles are common, but the help he has received is rare. As U.S. deaths from both legal and illegal opioids exploded from 9,489 in 2001 to 47,600 in 2017, the country began a widespread crackdown on the prescription painkillers. Health authorities, insurance companies, medical groups and even pharmacies began cutting off patients and sharply limiting dosages. The restrictions have caused anguish among the seven million to 10 million people who take these medications for chronic pain that stems from conditions ranging from fibromyalgia to spinal cord injuries to tissue damage left by war wounds or surgery. Even though illegal drugs (especially illicit fentanyl) cause the majority of overdoses, policy makers were alarmed that more than a third of opioid deaths involved prescription pills. In 2016 the Centers for Disease Control and Prevention issued a guideline, reminding doctors that the drugs should be used only as a last resort for chronic pain. It cautioned against prescribing daily doses above 50-milligram morphine equivalents (MMEs are a way to equate the doses of various opioids). States also jumped into action. At least 36 issued policies or guidelines that in some way limited the amount of opioids that doctors could prescribe. In addition, many doctors misconstrued the CDC guideline as a hard limit on dosage—even for long-term users. By 2017 almost 70 percent of family medicine physicians had cut back on prescribing the drugs, and nearly 10 percent stopped offering them altogether, according to a Boston Globe survey.
Abruptly cutting off patients, however, is a dangerous practice that can cause their pain to spike and lead them to turn to street drugs or suicide, experts warn. “It creates intense destabilization, both medically and psychologically,” says pain psychologist Beth Darnall of the Stanford University School of Medicine. She was among 92 experts and advocates who wrote an open letter in September 2018 to the federal Pain Management Task Force warning of “an alarming increase in reports of patient suffering and suicides.” Last April both the CDC and the Food and Drug Administration took action to warn doctors about these risks.
There is no question that cold-turkey cutoffs are bad, but sadly, there is a lot less clarity about how best to reduce opioid dependence among chronic pain patients. There never was much science to justify using these powerful drugs for months and years at a time and precious little to show how to reverse course. Fortunately, research, fueled by an influx of federal dollars, is beginning to point the way. Among the early findings: tapering long-term users appears to work best when done very slowly, with close individualized attention and instruction in alternative ways to handle pain—much the way Muccino has been helped. Surprisingly, some studies suggest that many patients wind up feeling better on lower doses or none at all, as side effects such as lethargy, mental fog and extreme constipation fade away. A new guide to dose reduction, issued last October by the U.S. Department of Health and Human Services (HHS), endorses these go-slow, collaborative, “patient-centered” techniques.
Many key questions remain the subject of ongoing studies, including such basic issues as when these drugs remain appropriate for chronic pain and at what doses, who truly needs to be tapered from opioids, and how best to go about it when patients are reluctant and fearful. “The pain research question that probably has the biggest impact on society right now is: What is the long-term safety and effectiveness of opioids?” says Sean Mackey, chief of the division of pain medicine at Stanford. “The reality is, we don’t know.” But slowly and surely, answers are arriving to safely unwind the great American love affair with opioids.
The Opioid Attraction
The idea that opioids are an appropriate choice for pain that is chronic—lasting more than three months—took off in the mid-1990s. It was a period when the medical community had begun to take pain more seriously in general, labeling it “the fifth vital sign” (after blood pressure, pulse, respiratory rate and temperature). It was also when OxyContin, an extended-release version of the opioid oxycodone, was introduced with much fanfare, along with some seriously misleading claims about its long-term safety and nonaddictive nature—claims that later became the subject of multimillion-dollar lawsuits. Prior to that, natural opiates such as morphine and synthetic opioids such as oxycodone were mainly used for acute short-term pain, cancer and palliative care. According to a CDC analysis, prescriptions for opioids quadrupled between 1999 and 2010.
The drugs were seen as a cheap alternative to the gold-standard treatment for intractable chronic pain: interdisciplinary pain-management and rehabilitation programs that involve a team of psychologists, doctors, physical and occupational therapists, and other specialists working with a patient over several weeks at specialized clinics. That approach is far more labor-intensive than taking a pill, but it addresses the “biopsychosocial” nature of chronic pain—the fact that what an individual feels is not wholly determined by the firing of pain nerve fibers but can be affected by mood, personality, social context and even the meaning a person attaches to pain. “If your pain means your cancer is getting worse, it’s much less tolerable than if it means you’ve trained hard for the marathon or you’re having a nice baby,” observes Mark Sullivan, a psychiatrist at the University of Washington’s Center for Pain Relief in Seattle.
Even though opioids were suddenly being prescribed en masse for people with bad back pain and all manner of long-term conditions, most studies had looked only at their effects over six weeks or less. That clearly was not enough time to observe the physical and psychological dependences that develop over months and years or how, as the body habituates to the drugs, people often require higher amounts that raise the risk of respiratory problems, dizziness and life-threatening overdoses.
A few doctors, at the time, were bothered by the knowledge gap. Opioid researcher Erin Krebs was in medical school in the mid-1990s. She remembers being surprised and skeptical that drugs that had never been studied over the long term were being prescribed for months and years at a time. Krebs, now chief of general internal medicine at the Minneapolis VA Health Care System, is researching ways to help the so-called legacy patients of the opioid era manage pain with safer doses. But she is also investigating the more basic question of whether opioids are ever a valid choice for long-term pain. Last year she published the first randomized trial to directly compare opioids with nonopioid painkillers—ranging from popular anti-inflammatories such as ibuprofen to nerve pain drugs such as gabapentin—during a full year. Her team followed 240 patients with moderate to severe back or joint pain and found that, on average, the nonopioid group reported less intense pain and fewer side effects. When she proposed the study in 2010, Krebs says, “the assumption was so strong that opioids were better, some people felt it would be unethical to say some patients couldn’t get opioids!”
Krebs has since found further evidence that opioids can be a poor choice for chronic pain. At a 2018 pain conference she presented some shocking preliminary data from a long-term study of 9,245 veterans taking opioids for six months or more. Only a quarter of participants rated the effectiveness of their pain treatment as very good or excellent, and 80.9 percent said that their pain was throughout their body—a symptom that might reflect a suspected drug side effect: a pain syndrome called opioid-induced hyperalgesia. “My initial impression was just wow,” Krebs told me. “These people are really sick. We have not fixed these folks.”
How to Cut Back
When the risk of opioids seems greater than the benefits—if patients are misusing the drugs or show overdose-related symptoms, for example—the new HHS guidelines urge doctors to consider tapering. The central questions then become how to do that without triggering more agony and desperation and what to offer for pain relief instead. In an ideal world, patients with intractable suffering would go to the interdisciplinary pain and rehabilitation clinics, which have a good track record of switching patients from opioids to other ways of managing pain. But many of these clinics closed when the medical community embraced opioids, and treatment at those that remain is costly. So the search is on for cheaper, practical approaches. In 2018 Darnall published one of the first papers to provide an answer: a very slow, personalized dose reduction.
In a pilot study with 68 patients published in JAMA Internal Medicine, Darnall showed that over the course of four months, the 51 individuals who completed the trial were able to cut their opioid dosages nearly in half, on average, without worsening pain. They received careful guidance from a community doctor and a self-help book. A slow reduction was especially critical during the first four weeks, she says, when the dosage was cut by no more than two 5 percent increments. That is considerably less than the 10 percent a week originally suggested in the CDC’s 2016 “pocket guide” to tapering opioids and in line with the HHS’s updated version.
“If we do these microdose reductions, it allows patients to relax into the process, to gain a sense of trust with their doctor and also with themselves,” Darnall explains. “Their number-one concern is increased pain.” The goal, she emphasizes, was not to get to zero but to “the lowest comfortable dose.” Four participants did manage to taper off completely, she says, “but four people didn’t budge or actually increased their dose,” and 17 dropped out of the trial. Notably, there was no correlation between a patient’s dose at the start of the trial or how long the person had been taking opioids and his or her ability to cut back.
Darnall is eager to determine if additional tools might help more patients succeed in tapering. With funding from the Patient-Centered Outcomes Research Institute (PCORI), an agency created by the 2010 Affordable Care Act, she is now overseeing a one-year trial with 1,365 chronic pain patients called EMPOWER (for Effective Management of Pain and Opioid-Free Ways to Enhance Relief). Five hundred of the patients do not wish to taper and will stick with their current opioid treatment, serving as a control group. The others will be randomly assigned to one of three treatments. One group will simply repeat the methods of Darnall’s pilot study. Another will do that regimen plus get eight weekly sessions of group cognitive-behavioral therapy (CBT) for pain, a type of short-term psychological counseling that focuses on changing patterns of thoughts and beliefs to affect behaviors and feelings. The third group will also follow the pilot protocol and add six weekly group workshops on pain “self-management.”
Pain self-management is a low-cost intervention led by trained peers rather than health professionals, but it has never been studied in the context of opioid tapering. The method, developed by Stanford health educator Kate Lorig, takes participants through a highly structured series of activities, lessons and discussions that offer tools for managing pain and reclaiming a more active life. At a typical session, patients make weekly “action plans” to do something they have been avoiding because of pain, such as taking a daily walk or cleaning out a closet, and report back on their progress. They learn exercises to warm up achy joints and brainstorm better ways to communicate with doctors. Participants say that being with others who understand chronic pain—including the group leaders—provides inspiration, support and accountability. “You realize that everyone is in a similar boat, and that helps,” says Sylvia Nomikos, a retired teacher with severe spinal stenosis, who attended a self-management workshop in Pleasantville, N.Y. Two studies of this type of intervention have found that participants report lasting reductions in pain, disability, depression and health-related anxiety.
Darnall’s team will assess how the pain self-management method stacks up against costlier CBT in her EMPOWER study and whether either improves on the basic, slow-tapering protocol. Along the way, they will also collect data on participants’ use of marijuana and cannabis products to see what impact they have on opioid reduction, and vice versa. The need for such research is pressing, Darnall says. No matter which interventions come out on top, if the outcomes for any group match or exceed those of her pilot study, she will have demonstrated a safe, practical and economical way to taper opioids that could be carried out in communities everywhere.
Easing Withdrawal
Other researchers, including Sullivan and Krebs, are also testing practical, low-cost ways to help pain patients reduce their reliance on opioids that, if successful, could be scaled up to meet the country’s huge need. Krebs is leading a large trial, also funded by PCORI, in which 500 U.S. veterans will work by phone with a pharmacist to optimize the safety and efficacy of their drug regimen. Another 500 will be assigned to a multidisciplinary team (a physician, psychologist and pharmacist or physical therapist) that will put less emphasis on meds as the solution and focus more on achieving personal goals and a better quality of life even if their pain cannot be cured. The study will also look at the usefulness of a medication designed to ease withdrawal.
“No one is required to taper in this study,” Krebs points out, but participants who are on high doses of opioids will be educated about their risks. Those who opt to taper will be randomly assigned to do so with or without the help of buprenorphine-naloxone (the generic version of Suboxone), a medication that combines an opioid painkiller with an opioid blocker and provides pain relief, reduces symptoms of withdrawal and has a relatively low risk of overdose. “We know this medication works in the opioid-addiction setting,” Krebs explains, “so we’re wondering if it could also help people in a pain-treatment context.”
The Opioid Reassessment Clinic in West Haven, where Muccino gets treatment, is a site in Krebs’s study. Its director, Will Becker, routinely offers buprenorphine-naloxone to patients to help trim their opioid use. About two thirds say yes, Muccino among them. Becker believes the drug provides “a soft landing” to people who have been opioid-dependent for years and years. He also thinks that just presenting patients with choices makes a big difference in their ability to taper: “Having an option empowers them.”
Opioid tapering at Becker’s clinic emphasizes achieving functional goals defined by patients. These could be returning to work or just getting out of bed earlier. “We try to target SMART goals: specific, measurable, action-oriented, realistic and time-bound,” Becker explains. “These are discrete, real things that they can reengage with—things that pain has taken away.”
For Muccino, a major goal was to enjoy time with his seven grandkids or, as he put it, “being able to see my grandchildren grow as long as I can—through clean eyes.” He regrets missing much of his own kids’ childhood: “I was working 60 to 70 hours a week, and I was high on drugs. I’d come home and pass out on the couch.” Using buprenorphine-naloxone under Becker’s supervision helped him stop taking the OxyContin entirely.
A handful of studies and clinical experience suggest that once patients get past their initial fears, many feel better on lower doses or leaving opiates behind. The underlying pain will not necessarily change, says Stanford’s Mackey, but on low doses “what I see is they feel more alive, alert and aware.” This is presumably because opiate compounds—including those made in our own bodies—work on several systems in the brain, including those that regulate emotions and attention. “When you flood those systems [with drugs], you get blunted over time.” Still, there is a minority of patients who do worse, and pain specialists worry about this group, especially at a time when patients are being pressured to cut back. They point out that not everyone can be weaned or even tapered from opioids, and not everyone should be [see “When to Stick with Opioids” below].
Beyond Opioids
The path away from opioids is going to mean starting fewer patients on them to begin with and making other treatments more accessible—including physical and behavioral therapies and scores of nonopioid medications that are used to fight pain. The first part is easier and already happening: a large study published last year found that first-time opioid prescriptions fell 54 percent between July 2012 and December 2017. What’s harder is changing medical practice and patient expectations about what chronic pain treatment looks like. As Sullivan observes, “There’s no better way to make your patient happier than to give him some OxyContin, because he feels better in the car on the way home from the pharmacy.” Other therapies, he notes, tend to take effect more slowly: “they can make you feel worse before they make you feel better. They can be a lot of work,” as is the case with physical or behavioral therapy.
It would help if doctors, especially those in primary care, got better training in how to assess and treat pain, an issue noted by the federal National Pain Strategy released in 2018. (U.S. medical students get only four to 12 hours of instruction on pain, according to a 2011 survey. Veterinarians, by comparison, get 28 hours, Darnall says.) The strategy also points out that “the public at large” would benefit from a better grasp of pain’s complexity and how to manage it.
Muccino has gained that understanding. These days, in addition to a low dose of buprenorphine-naloxone, he manages his pain with relaxation, distraction and methods he learned in CBT. At home, he pipes some James Taylor songs through his earbuds, stretches and strengthens with physical therapy exercises. He counts himself lucky to have a supportive family so when the going gets rough, he says, “I play with my grandkids. I go for a ride. Anything but take a pill.”
When to Stick with Opioids
While researchers are determining how best to wean pain patients from high-dose opioids, it is quite clear that not everyone can or should cut back. The CDC has explicitly exempted people in pain from cancer or sickle-cell anemia from its cautions about prescribing the drugs. In addition, experts will often hesitate to mess with patients who are living with such profound pain that their lives are balanced on a knife’s edge. Andrea Anderson, a patient advocate who was executive director of the Alliance for the Treatment of Intractable Pain, tells story after story of people in extremis—a man who survived 20 minutes of electrocution, a patient who had been engulfed in flames— who depend on large quantities of opioids but who do not dare to taper. No one should be forced to, experts agree.
Clinicians also have seen patients who remain stable and functional on a steady dose, holding down jobs, taking care of their families, not escalating their dosage. “We’ve got guys who stay on 15- to 20-milligram morphine equivalents [MMEs] for years and do well,” says Will Becker, who directs the Opioid Reassessment Clinic at the VA Medical Center in West Haven, Conn., although he concedes that “I’ve seen a whole lot more who have not stayed on low doses and do poorly.”

The thorniest questions arise for patients who are on high doses, continue to struggle with pain and an overall poor quality of life, but do not wish to taper. Often these patients are medically complex, with a variety of physical or psychological conditions that make it difficult to tease apart what portion of their pain is caused by an underlying biological issue, what is the result of drug side effects, and what stems from other ailments that afflict them. “This is where we get into the gray zone,” says Sean Mackey, who heads the division of pain medicine at Stanford University. “We need to personalize the approach to each patient and work collaboratively. There is not a one-size-fits-all here.”
Not all patients do well with tapering, even if it is done slowly and carefully. Take Nadine Hagl, a 53-year-old army veteran who was referred to Becker’s clinic after many years on high-dose Percocet (an oxycodone-acetaminophen combo). Hagl is medically complex in several ways. In addition to painful arthritis that leaves her reliant on a cane, she suffers from PTSD and used to carry 240 pounds on her 5-foot, 1-inch frame before undergoing gastric bypass surgery in 2014 and losing 130 lbs. Her rerouted gut cannot tolerate nonsteroidal antiinflammatory painkillers, which might otherwise be an alternative to opioids, nor does she respond well to buprenorphine, a medication used to mitigate opioid withdrawal. Hagl is psychosocially complex, too, given her PTSD diagnosis and the fact that she is the single mom of a son who is on the autism spectrum. Working with Becker’s team, Hagl made a good faith effort to try a number of alternatives to opioids, but her pain flared up. They agreed to return her to Percocet, along with an array of nondrug therapies, but specified a lower dose than before and close monitoring.
Pain and addiction specialists agree that patients who remain on long-term opioids should be monitored carefully for side effects and for signs of abuse. All 50 states have prescription-monitoring programs that enable clinicians to detect if a patient is double-dipping with another prescriber and putting themselves at risk.
Given all the pressures to reduce opioid use, it is likely that the number of people taking these drugs long term will continue to dwindle. Mark Sullivan, a pain psychiatrist at the University of Washington, remembers the sparing use of these narcotics that prevailed when he entered the field 30 years ago. “I think we will get to the point where, as it was when I started, opioids are very useful and should be used short term and long term only in exceptional circumstances.”
— C.W.