Why sleep has restorative—or damaging—effects on cognition and brain health has been an enduring mystery in biology. Researchers think cerebrospinal fluid (CSF) may flush toxic waste out, “cleaning” the brain and studies have shown that garbage clearance is hugely improved during sleep. They were not sure exactly how all this works, however, or why it should be so enhanced during sleep.
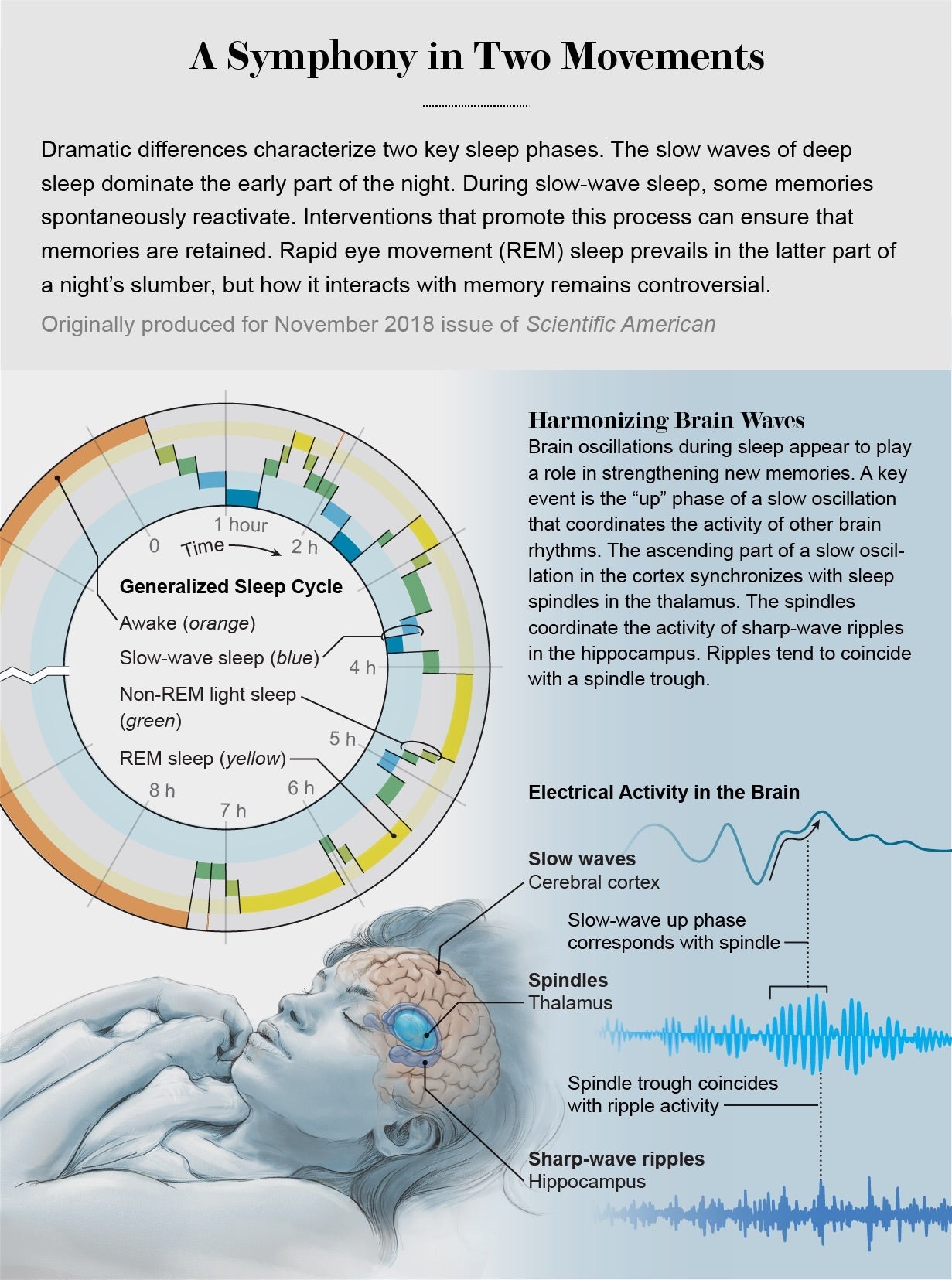
One aspect of sleep that is well understood is how the slow electrical oscillations (or “slow waves”) that characterize deep, non-REM sleep contribute to memory consolidation, the process whereby new memories are transferred into long-term storage. A new study, from a team led by neuroscientist Laura Lewis of Boston University, now gives insight into what drives CSF flow through the brain, suggesting that the same slow waves that coordinate memory consolidation drive oscillations in blood flow and CSF in the brain.
The work has implications for understanding the relations between sleep disturbance and psychiatric and neurodegenerative conditions, and may even point to new approaches to diagnosis and treatment. “We’ve discovered there are really large waves of CSF that appear in the brain only during sleep,” Lewis says. “This effect is really striking, and we’re also interested in what it means for maintaining brain health, especially in disorders such as Alzheimer’s disease.”
In the study, published on October 31 in Science, the team set out to investigate how the dynamics of CSF flow changes during sleep, and how this might relate to alterations in brain blood flow and electrical activity. “We know sleep is really important for brain health, and waste clearance is probably a key reason why; what was less clear is: Why is this changed during sleep?” Lewis says. “That led us to ask what was happening in the CSF.”
The researchers used electroencephalography (EEG) to monitor the brain waves of 13 sleeping healthy adults, while also using a cutting-edge, “accelerated” fMRI technique to capture faster changes than standard fMRI can manage. That allowed for the measurement of both blood-oxygenation changes (which indicate blood flowing to electrically active, oxygen-hungry regions) and CSF flows. The latter was only possible due to a flaw in this method that means any newly arriving fluid (not just oxygenated blood) lights up in the image. “We realized we could take advantage of this to measure CSF flow at the same time as blood oxygenation,” Lewis says. “That was critical, because it turns out these things are coupled to each other in a way we never would have seen if we didn’t measure blood, CSF and electrical activity simultaneously.”
What the team found was that the slow waves seen in non-REM sleep occur in lockstep with changes in both blood flow and CSF. Just because things occur together doesn’t necessarily mean one causes the other, but the team also built a computer model incorporating what we know about the physics linking these processes, which predicted that slow waves would have just these kinds of effects on blood and CSF. What seems to be happening is that as brain activity alters blood flow, this reduces the volume of blood in the brain, and because the brain is a closed vessel, CSF flows in to fill the space. “It’s very convincing,” says neurologist Maiken Nedergaard of the University of Rochester, who was not involved with the research. “It also really makes sense: electrical activity drives blood flow changes, that then drive CSF changes.”
The team measured this CSF inflow going into the fourth ventricle, one of four fluid-filled cavities involved in producing CSF (by filtering blood plasma) and circulating it around the brain. As CSF usually flows out of the fourth ventricle, this suggests a “pulsatile” flow, like a wave. This pushes CSF around the ventricles and into spaces between membranes surrounding the brain and spinal cord, called the meninges, where it mixes with “interstitial fluid” within the brain to carry away toxic waste products.
As slow waves are important for memory consolidation, this links two disparate functions of sleep. “What’s exciting about this is it’s combining features of brain function that people don’t normally think of as connected,” Nedergaard says. It isn’t obvious things had to be this way, Lewis says, but it may represent an example of nature being efficient. “It’s a matter of nature not dividing tasks between higher level and lower level, like how you run a company, where you have a boss making decisions and cleaning people coming in,” Nedergaard says. “In biology, it’s everybody contributing, as it makes more sense.”
The findings have implications for neurodegenerative diseases, which are thought to be caused by build-up of toxic proteins in the brain, such as amyloid-Beta in Alzheimer’s disease. Previous research has shown that amyloid-Beta is cleared more efficiently during sleep, which is often disrupted in patients. Disturbances in slow-wave sleep also often accompany aging, which may be linked to cognitive decline. “We know that people with Alzheimer’s have fewer slow waves, so we may find they also have fewer CSF waves,” Lewis says. “We have to do these studies now in older adults and patient populations, to understand what this might mean for those disorders.” Sleep disturbance is also a feature of many psychiatric disorders, from depression to schizophrenia. “Different electrical signatures of sleep are disrupted in different psychiatric conditions,” she says. “So this will be very interesting to follow up on in a multitude of disorders.”
The team next hope to nail down whether electrical oscillations truly do cause the changes they observed in CSF flow, by experimentally manipulating brain activity. “It would be great to find the right collaborator and do a study in mice where we manipulate neural activity, then watch the downstream consequences,” Lewis says. “We’re also thinking about ways to safely and noninvasively manipulate neural oscillations in humans.” It may ultimately be possible to use electromagnetic stimulation to influence brain waves as a treatment for brain disorders. Researchers have already seen encouraging results of this approach in mice, and these findings may help explain why. Another potential application may come from assessing whether changes in CSF flows can serve as a diagnostic marker for some of these conditions. “It gives us a ton of interesting new biology to explore and understand, since it seems like things the brain is doing during sleep are related to each other in surprising ways,” Lewis says. “Maybe the most important take-home message is that sleep is a serious thing,” Nedergaard says. “You really need to sleep to keep a healthy brain because it links electrical activity to a practical housekeeping function.”


