One of the many issues that have flummoxed scientists researching COVID-19 is the nose-to-toes diversity of its symptoms, which extend well beyond the usual range of respiratory infections: from loss of smell to blood clots and stroke to limb pain and discolored COVID toes. One of the most common nonrespiratory manifestations is gastrointestinal trouble. As many as 50 percent of COVID patients have nausea, diarrhea and/or abdominal pain. And according to a Canadian review paper, for 16 percent in one large study, those were the only symptoms.
Research indicates that SARS-CoV-2—the virus that causes COVID—can directly attack the epithelial cells that line the GI tract, entering via the molecular doorway of angiotensin‐converting enzyme 2 (ACE2). These cells express high levels of ACE2, as do the cells lining the lungs, the primary site of infection.
But the gut is not merely a passive target for the virus. Evidence suggests it is also a player in determining the severity of COVID-19. A burst of research over the past decade has shown that the tiny denizens of the digestive tract—the gut microbiota—play a vital role in protecting the body from pathogens and in regulating immune responses to infections, and that seems to be the case for COVID.
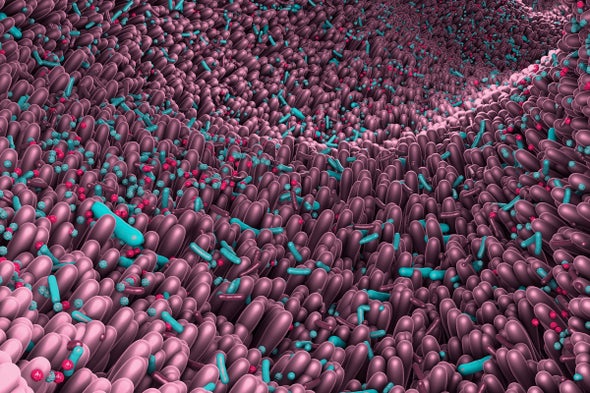
Trillions of bacteria, fungi, viruses and other single-celled organisms reside in the gastrointestinal tract in a dynamic, commensal ecosystem. And each of us harbors our own unique community. When our gut microbiota are in a diverse but healthy and balanced state, they support the proper functioning of our immune system. When the balance is perturbed—a condition scientists call dysbiosis—our defenses are compromised, and we are more susceptible to infections.
The diversity of the gut microbiota is known to decline with increasing age. And similarly, there is an association between altered gut microbiota and chronic diseases, such as obesity, diabetes and cardiovascular disease—conditions that predispose individuals to severe COVID-19. There isn’t yet proof of a direct relationship between COVID severity and gut dysbiosis, but evidence is mounting.
In a 2021 study of 100 patients hospitalized with COVID, Siew C. Ng and her colleagues at the Chinese University of Hong Kong found that, overall, the subjects’ gut microbiome (as measured in stool samples) was significantly less diverse than samples taken from a prepandemic control group, regardless of whether the patients had taken antibiotics or other drugs. A number of beneficial bacterial species were deficient in COVID patients, and the degree of microbiome disturbance correlated with disease severity and increased signs of inflammation.
“Several gut microorganisms with known immunomodulatory function were depleted in patients with COVID-19,” Ng explains. Their depletion might be a factor in the “cytokine storm,” the dangerous, hyperinflammatory state that is sometimes seen in COVID patients, says Ng, who is associate director of the Chinese University of Hong Kong’s Center for Gut Microbiota Research.
That scenario is one of several ways in which our gut residents could influence COVID severity. The precise mechanisms are not yet known, “but we can hypothesize,” says Harry Sokol, who studies the relationship between gut microbes and the immune system at Saint-Antoine Hospital in Paris. He suggests that “in the early phase of infection, there is an alteration of the gut microbiota leading to a decreased production of microbiota-derived [substances] that are important to control the infection.” Such changes were observed in a 2021 study led by Sokol in which macaques were infected with SARS-CoV-2.
In a later phase of COVID, Sokol suggests, the decline in certain microbes might impact the integrity of the gut. These microbes normally generate substances that help maintain the gut lining, including short-chain fatty acids such as butyric acid. Lower levels of key bacteria might therefore cause a “leaky gut,” which, in turn, could cause pro-inflammatory molecules to leach out, ramping up cytokine storms that can cause the extensive organ damage seen in severe COVID cases.
Damage to the gut itself—and to other organs—may be the result of inflammation, the viral attack itself or the disruption of ACE2’s normal functions. In the gut, ACE2 plays many roles including regulating the ecology of the gut microbiota. Thus, it is not clear if COVID causes an unhealthy gut or if an unhealthy gut sets the stage for severe COVID. “Probably both are true and linked,” Sokol says.
Gut microbes may influence COVID outcomes through an exchange of chemical signals with cells in the lungs. This recently discovered “gut-lung axis,” like most biological axes, is a two-way affair: intestinal microbes influence how the lungs respond to infections, and lung inflammation can also alter the gut microbiota. For example, a review study by Brazilian scientists that was published earlier this year found that research showed that chemical signals sent by gut bacteria and received by cells in the lungs can help protect mice from infection with an influenza virus, whereas giving mice antibiotics that disrupt their gut microbiota compromises their immune response to influenza. If the same is true for COVID in humans, clinicians should be cautious about using antibiotics in COVID patients—unless, of course, they have secondary microbial infections.
As scientists learn more about the role of the gut in COVID, there may be other implications for treatment and prevention. Monitoring gut health may be one way to predict severity, and using probiotics and improved diet to boost the microbiome might prove to be a valuable strategy. Ng notes that several randomized trials with a specially formulated mix of probiotics are underway at her institution: these trials aim to reduce the risk of COVID in vulnerable groups such as the elderly and people with diabetes and to improve response to COVID vaccines. Other researchers are also testing the possible benefits of using probiotics and of transplanting fecal organisms to COVID patients with deficient gut populations.
There may even be lessons for the dreaded “long COVID.” In their 2021 study, Ng and her colleagues found that gut dysbiosis persisted in many recovered COVID patients when the virus was no longer detectable and that it could contribute to ongoing health problems. The study followed some patients for 30 days after recovery, and the authors believe longer follow-up of this issue is warranted. It may be advisable, Ng says, for “recovered patients to consume diets or incorporate activities known to be good for the gut microbiome: increasing fiber intake, taking probiotics and exercising.” It’s sound advice under any circumstance.
This article is part of an editorially independent Springer Nature collection that was produced with financial support from Lonza.