Millions of people have been pregnant and given birth during the pandemic. When the COVID-causing virus SARS-CoV-2 first emerged, it wasn’t clear what additional risks—if any—it posed to pregnant people and their babies.
But accumulating evidence now shows that having COVID during pregnancy increases the likelihood of severe outcomes and death in the parent, as well as the possibility of fetal complications. A large meta-analysis published in BMJ in January found that pregnant women infected with the virus have a significantly higher risk of complications, including pneumonia, intensive care unit admission, mechanical ventilation and death, compared with uninfected pregnant women. And babies born to infected women were more likely to be admitted to a neonatal intensive care unit (NICU), to be born preterm or to have a low birth weight.
“There are two reasons you can be really sick in pregnancy” with a COVID infection, says Emily Smith, an assistant professor of global health at the George Washington University Milken Institute School of Public Health and lead author of the meta-analysis. “One [is] from COVID itself—pneumonia and other things that any person [could] have from COVID. And…it may cause or exacerbate existing maternal morbidities—things that any pregnant person could have.”
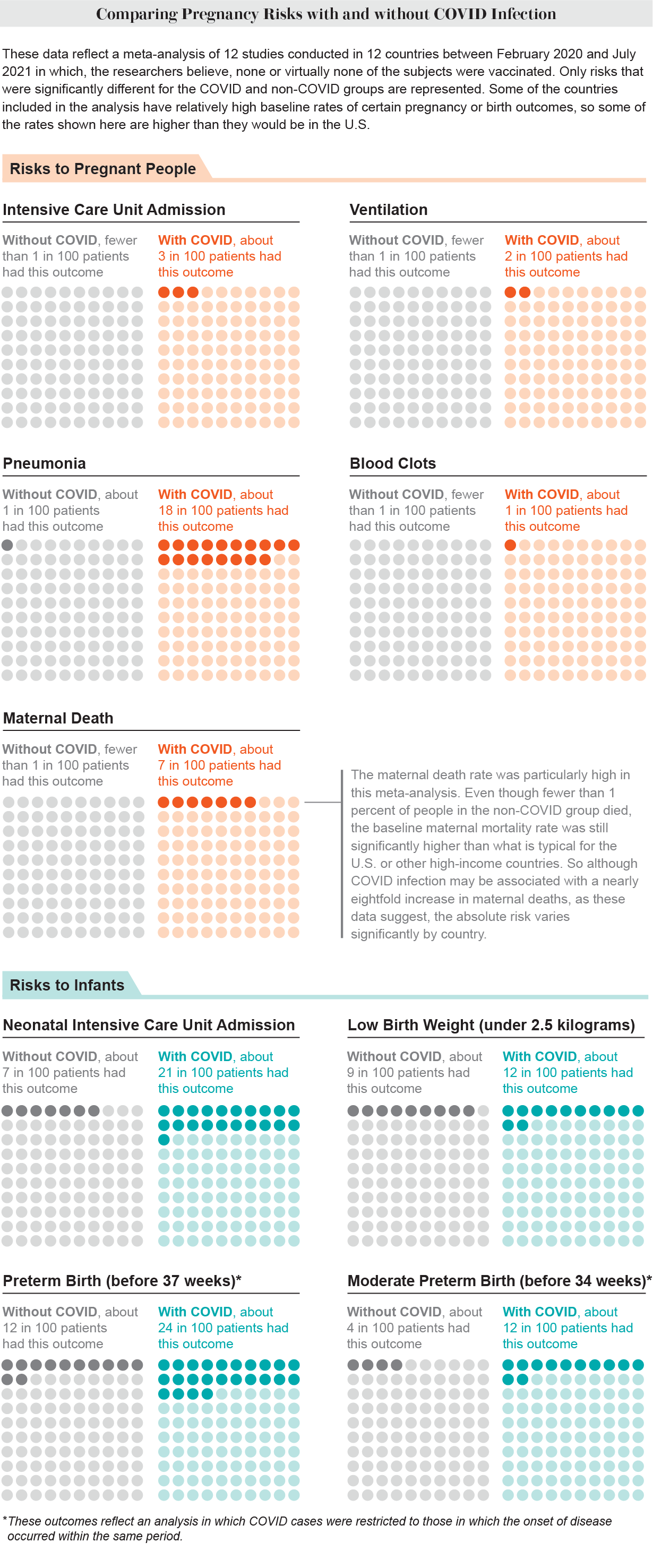
Credit: Amanda Montañez; Source: “Adverse Maternal, Fetal, and Newborn Outcomes among Pregnant Women with SARS-CoV-2 Infection: An Individual Participant Data Meta-Analysis,” by Emily R. Smith et al., in BMJ Global Health, Vol. 8, Article No. e009495. Published online January 16, 2023
Fortunately, vaccination mitigates many of these risks. A study published in the February 11 issue of the Lancet found that vaccinated pregnant women were are at lower risk of severe COVID, ICU admission and death than unvaccinated pregnant women. And if they received a booster shot, the risk was even lower.
“Because pregnant women are generally young and fit and healthy, they don’t consider themselves to be at a high risk,” says the Lancet study’s senior author Aris Papageorghiou, a professor of fetal medicine and director of research at the Oxford Maternal & Perinatal Health Institute. “But the truth of the matter is that when you are pregnant, you are at higher risk from COVID infection.”
It is well established that flu and other infections are more dangerous during pregnancy. There are possible reasons for this. One hypothesis is that pregnant people experience immunological changes that prevent their body from rejecting the fetus—much like it might reject a transplanted organ, Papageorghiou says. Another reason, he adds, could be that the growing uterus puts pressure on the lungs, making it harder to breathe. Additionally, some pregnant people may be undertreated for an infection because doctors are nervous about drugs’ effects on the fetus, Smith says.
Early in the pandemic, Smith and her colleagues sought to quantify the risks COVID posed to pregnant people and their babies. The researchers started collecting data in April 2020, and their analysis ultimately drew on 12 studies that involved a total of more than 13,000 pregnant women. These studies were conducted between February 2020 and July 2021 and spanned 12 countries: Ghana, China, Italy, Kenya, Nigeria, South Africa, Spain, Sweden, the Democratic Republic of the Congo, Turkey, Uganda and the U.S. In most of the studies, COVID was diagnosed with a PCR test. Importantly, it was likely that virtually none of the women in the study were vaccinated, as most of the data were collected before vaccines were widely available or in places with low uptake, Smith notes.
The results showed that, on average, pregnant women with COVID had a greater than sevenfold risk of death, compared with pregnant women who did not have it. Only three of the 12 studies recorded deaths, however. And while the study found that the absolute risk of pregnant women dying from COVID was relatively high—seven deaths per 100,000 pregnant people diagnosed with the disease—it’s important to note that some of the countries where the studies were conducted have much poorer maternal health care than the U.S. (meaning that this death rate is not representative of all women, especially in wealthy countries such as the U.S.). Nevertheless, the risk was still found to be significantly increased.
Pregnant women with COVID were also 23 times more likely to develop pneumonia, 15 times more likely to need to be put on a ventilator, more than five times more likely to have blood clots and nearly four times more likely to be admitted to an ICU while pregnant.
Furthermore, babies whose mothers had COVID were nearly twice as likely to be admitted to a NICU, 1.7 times as likely to be born preterm and slightly more likely to have a low birth weight. The researchers did not find an association between COVID infection in the mother and stillbirth.
“The big takeaway for me is that these are serious consequences for mom and for baby, and these are big risks,” Smith says. “On the other hand, don’t panic. But it is a reason to take some precautions to protect yourself.”
The findings add to those of a previous study that was published in 2021 in JAMA Pediatrics by Papageorghiou and his colleagues. It, too, found that pregnant women and their babies were at an increased risk of severe complications and death from COVID.
Yet there is now increasing evidence that vaccination protects pregnant people from the worst COVID outcomes.
In their Lancet study earlier this year, Papageorghiou and his team analyzed about 4,600 pregnant women during the period when the first Omicron variant of SARS-CoV-2 was circulating (late November 2021 through June 2022). The researchers found that COVID vaccination with the primary series alone was 48 percent effective at protecting against severe disease in all pregnant women, and vaccination followed by at least one booster was 76 percent effective. For pregnant women who actually got COVID, vaccination with the primary series was 74 percent effective against severe disease, and with the booster, it was 91 percent effective.
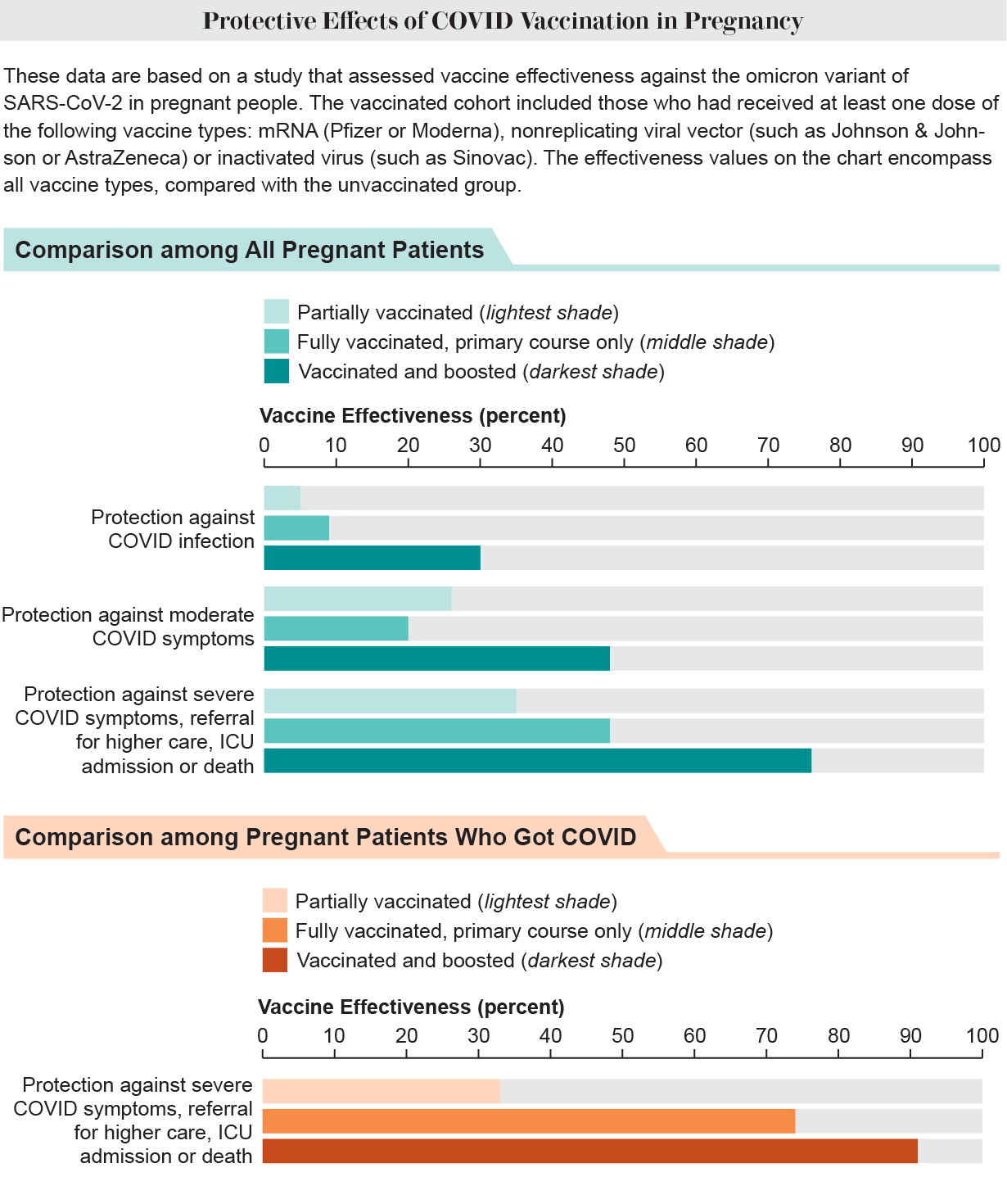
Credit: Amanda Montañez; Source: “Pregnancy Outcomes and Vaccine Effectiveness during the Period of Omicron as the Variant of Concern, INTERCOVID-2022: A Multinational, Observational Study,” by José Villar et al., in Lancet, Vol. 401, No. 10375; February 11, 2023
“Almost all the adverse effects were in women who had not been vaccinated. Vaccines still provided a very powerful reduction in maternal morbidity,” Papageorghiou says. “Women with boosters had more protection than women who hadn’t had a booster. And women who had a vaccine within the last 10 months were much less likely to have [severe] symptoms.”
Asma Khalil, a professor of obstetrics and maternal-fetal medicine at St. George’s Hospital at the University of London, and her colleagues have also found that in pregnant people, the vaccine was nearly 90 percent effective at preventing SARS-CoV-2 infection a week after the second dose—though protection likely declines over time. Those vaccinated also had a 15 percent lower risk of stillbirth. (Vaccination was not associated with significantly lower risk of miscarriage or fetal abnormalities, however.) “We have reassuring data from a large number of pregnant individuals that the vaccine is effective and safe,” Khalil says, and that “the vaccine is protective of the mother and the baby.”
Other studies have found that the antiviral medication Paxlovid can be safely given to pregnant people at high risk of developing severe COVID (for reasons unrelated to the pregnancy).
When the COVID vaccines first became available, a number of those who were pregnant felt hesitant about getting the shots because the vaccines’ clinical trials did not explicitly recruit pregnant people. Yet some of the people in the trials did become pregnant, and there was no evidence of adverse effects from vaccination, Papageorghiou says. “When we look at those [data], there were no excess miscarriages, there were no differences in fertility rates,” he says, adding that the U.S. vaccine surveillance system—which tracks adverse events from vaccination—has reported no congenital problems or problems with fetal growth.
Given the measurably greater risks pregnant people face from COVID infection and the safety and efficacy of vaccination, the main challenge may be persuading more pregnant people to get vaccinated. Health care providers such as midwives and ob-gyns have a role in educating their patients. “All we can do is just inform women with the best information,” Papageorghiou says. “Give them the facts.”