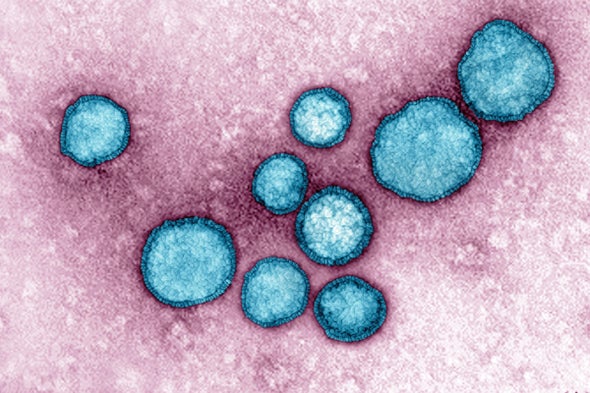
Every autumn, doctors’ offices, hospitals and clinics fill with babies and toddlers struggling to breathe. Families are frightened and bewildered as young children cough, wheeze and become increasingly congested, dehydrated and short of breath. Those of us who care for children know this means the annual epidemic caused by respiratory syncytial virus, or RSV, has started.
The recent RSV surge, has overwhelmed emergency departments, pediatric inpatient wards and intensive care units worldwide. Doctors and nurses are treating children in makeshift tents or improvised waiting areas in places around the U.S., and exhausted health care workers struggle to care for children so sick they can’t even catch their breath. At Seattle Children’s Hospital, where I’m a specialist in pediatric infectious diseases, we have declared our situation a “crisis” as we see patient volume surge in our emergency department at rates beyond our capacity. After COVID isolation spared children for two years, the 2022 RSV outbreak has been the worst in many years, or perhaps ever.
In any given year, RSV is the single most common reason young children are admitted to most U.S. children’s hospitals, even more common than flu, yet some people have never heard of it. This virus can cause disease as severe as influenza in the very young and old.
Currently, we have no vaccine to prevent RSV. This may be partly why RSV is so unknown, as flu shot campaigns have made the influenza virus a part of our culture. We have only one preventative treatment for RSV that we save for the most vulnerable babies, a monoclonal antibody administered as a monthly injection during RSV season. After 60 years of disappointingly slow progress in preventing RSV, there is now reason to be optimistic that we will soon be able to prevent this frightening disease.
We first learned about RSV disease in the 1940s as an unidentified cause of hospital nursery outbreaks. Researchers first isolated the virus in the 1950s. We now know that RSV occurs annually in the fall in temperate countries worldwide, and that our immune response to RSV may not prevent reinfection even in healthy young adults. This virus really affects the most vulnerable—some young infants may get so tired trying to catch their breath, they simply stop breathing. It’s rare for children in industrialized countries to die from RSV, as we give them supportive care including oxygen, intravenous fluids and even mechanical ventilation. But in low- and middle-income countries, RSV-associated health problems and mortality remain high. About 97 percent of RSV-related deaths worldwide occur in young children living in developing nations, and about one in 28 deaths in infants between 28 days and 6 months of age in these countries is related to RSV.
A major advance in RSV clinical care has come with new rapid diagnostic tests. Until recently, we had to take nasal swabs and add them to cultured cells, waiting for up to a week to see changes caused by the virus. Today, molecular techniques similar to those we use to diagnose COVID can rapidly detect the virus. Unfortunately, unlike with COVID, we have no rapid at-home tests for RSV.
Doctors began using antibodies to protect young babies from RSV after researchers found that maternal antibodies that passed naturally from mother to baby prior to delivery could help prevent serious RSV disease in infants. Palivizumab, approved in 1998, is an engineered antibody we give to preterm and high-risk infants every month during RSV season. It’s expensive, so we use it on the highest-risk infants, and it’s not generally available in developing countries. Clinical trials of several new long-lasting antibodies are underway, with some completed, in both healthy and high-risk children, with the expectation that one shot will prevent RSV disease in infants for up to six months.
The first attempts to develop an RSV vaccine began with methods similar to that of making polio vaccine. The virus was grown in cells, and inactivated with formalin to make the “dead” virus stimulate an immune response without causing illness. Unfortunately, this formalin-inactivated (FI) vaccine ran into safety issues—doctors tested it in young children and the vaccine initially appeared safe although not protective against RSV. But the next year, many of the vaccinated children who were again exposed to RSV developed severe disease - two of them died. This unexplained “enhanced disease” related to infection after the FI vaccine halted RSV vaccine research for decades.
Over time, as the understanding of RSV improved due to advances in biomedical technology and research, we learned that, among other things, the immune system was likely creating poorly functioning antibodies in response to the FI vaccine. We also learned that the FI vaccine wasn’t correctly educating the immune system how to best neutralize the virus. When the children who received the FI vaccine contracted RSV the next year, their immune systems were not appropriately responsive to RSV. They produced a poorly functioning and poorly binding antibody that was cross-reactive to other proteins. It failed to clear the virus, causing inflammation, as well as a likely imbalance of certain immune cells, leading to more severe disease.
The way that humans respond to our first exposure to a virus or bacteria is an important step in educating the immune system, and now we better understand the type of response that is needed when we develop vaccines. More than 50 years later, these and many other studies have improved our understanding of RSV virology and immunology, and are helping us design new approaches to RSV disease prevention.
About 15 years ago, researchers made impressive gains in the understanding of the molecular structure and function of RSV proteins as well as antibodies, setting the stage for both developing better vaccines and creating biological products that produce high levels of protective antibodies. We have recently completed trials using new vaccines that target RSV proteins in pregnant women to protect women and babies. Using maternal immunization to prevent RSV is similar to the approach used for influenza, where boosting maternal antibody during pregnancy results in high levels of antibody transferred to the infant by the time of birth. In older people, early results from two large international multicenter, placebo-controlled trials of RSV vaccines show promising, but unpublished results.
The post-COVID RSV epidemics worldwide are creating more awareness of RSV. Federal and foundation funding for RSV research has been woefully inadequate throughout my career, and although this is now improving, we still need more funding for research and to assess how best to use the new RSV prevention approaches. Prevention in less-industrialized countries is a high priority because this is where disease burden is highest, but prevention to avoid overcrowded hospitals and clinics is also critical. The burden of annual RSV epidemics on our health care system is enormous and increasing. As a researcher who has cared for children and adults with RSV and studied RSV prevention for decades, I am hopeful these new approaches will help protect children and prevent future crises in clinics and hospitals.
This is an opinion and analysis article, and the views expressed by the author or authors are not necessarily those of Scientific American.
The author’s institution, Seattle Children’s Research Institute, receives research support from CDC, NIH, Gates Ventures, AstraZeneca, GlaxoSmithKline and Pfizer Inc. for RSV-related clinical studies, and the author serves as a consultant on RSV-related matters for AstraZeneca, Meissa Vaccines, Moderna and Sanofi Pasteur.