Psychotherapy is not what most people think of as a quick fix. From its early Freudian roots, it has taken the form of 50- to 60-minute sessions repeated weekly (or more often) over a period of months or even years. For modern cognitive-behavioral therapy (CBT), 10 to 20 weekly sessions is typical. But must it be so? “Whoever told us that one 50-minute session a week is the best way to help people get over their problems?” asks Thomas Ollendick, director of the Child Study Center at Virginia Tech.
For nearly 20 years Ollendick has been testing briefer, more intensive forms of CBT for childhood anxiety disorders and getting results that closely match those of slower versions. His center often has a waiting list for treatments that include a four-day therapy for obsessive-compulsive disorder (OCD) and a three-hour intervention for specific phobias (such as fear of flying, heights or dogs). Around the U.S. and Europe, short-course therapies for anxiety disorders have begun to catch on, creating a nascent movement in both adult and child psychology.
The idea originated with Swedish psychologist Lars-Göran Öst, now professor emeritus at Stockholm University. Some 40 years ago Öst got the impression that not all his phobia patients needed multiple weeks of therapy and decided to ask if they would like to try a single, three-hour session. His first taker was a 35-year-old spider-phobic woman. “She lived five hours away, so she was happy,” he recalls, to be treated in one go. He later showed the efficacy of the approach in a clinical trial, although it took four years to recruit 20 participants. “People with a specific phobia rarely apply for treatment,” he explains. “They adjust their lives [say, avoiding spiders] or think they can't be helped.” Öst went on to work with a team in Bergen, Norway, to test an intensive therapy for OCD known as the Bergen four-day treatment. By the early 2000s Ollendick was adapting brief therapies for adolescents and kids.
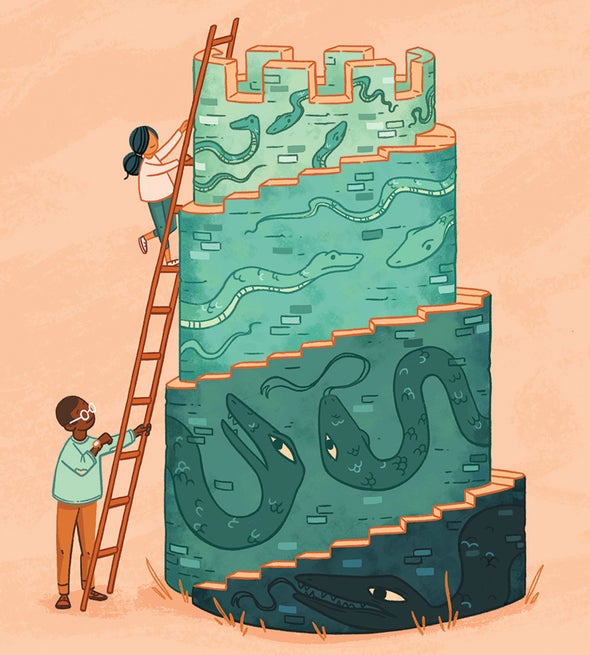
The details vary, but the quick treatments have some common features. They generally begin with “psychoeducation,” in which patients learn about their condition and the catastrophic thoughts that keep it locked in place. In Bergen, this is done in a small group. With children, the lessons may be more hands-on and concrete. For instance, Ollendick might help a snake-phobic kid grasp why the creature moves in a creepy, slithering way by having the child lie on the floor and try to go forward without using any limbs.
A second part usually involves “exposure and response prevention,” in which patients confront in incremental steps whatever triggers their anxiety: perhaps shopping, for agoraphobics, or having dirty hands, for people with OCD. With support from the therapist, they learn to tolerate it and see it as less threatening. Patients leave with homework to reinforce the lessons. Parents may be taught how to support a child's progress.
How well do these approaches work? A 2017 meta-analysis by Öst and Ollendick looked at 23 randomized controlled studies and found that “brief, intensive, or concentrated” therapies for childhood anxiety disorders were comparable to standard CBT. With the quicker therapies, 54 percent of patients were better immediately post-treatment, and that rose to 64 percent on follow-up—presumably because they continued to practice and apply what they had learned. With standard therapy, 57 percent were better after the final session and 63 percent on follow-up. The severity of symptoms and whether the patient was also taking antianxiety medication did not seem to impact outcomes.
An obvious advantage to quick therapy is that it accelerates relief. Children with panic disorder, for instance, may refuse to leave home for fear of triggering an episode of shortness of breath, a racing heart and nausea. “They start to avoid places like the mall, the movies, the school dance,” says child psychologist Donna Pincus of Boston University. Pincus developed an eight-day treatment for the disorder as an alternative to three months of CBT, which, she observes, “is a long time if you are not going to school or are avoiding doing things that are fun or healthy.”
Making these briefer therapies more widely available could help address the sad fact that only about a third of patients with anxiety disorders get any kind of treatment. A weeklong therapy could be completed over a school or work vacation. Rural patients who cannot find CBT nearby could be treated during a short out-of-town stay. The intensive approach requires special training and a big shift for therapists—and health insurers— accustomed to the tradition of 50-minute blocks. But is there really anything sacred about that?