In January 2020, news outlets around the world reported a disease outbreak in China caused by a new pathogen. For a while, the now all-too familiar disease called COVID-19 appeared to be mostly contained in China—at the start of the final week of January, there were 2,700 confirmed cases in the country and only around 40 cases elsewhere. The rest of the world scrolled past the headlines, failing to see what was coming.
Tom Inglesby, a physician and director of the Johns Hopkins Center for Health Security at the Bloomberg School of Public Health in Baltimore, Maryland, however, recognized some alarming signs in China. Health-care workers were becoming ill in large numbers; young, healthy people were dying; large temporary hospitals were being built, and officials ordered the shutdown of a city larger than any in the United States. Inglesby knew that disease spread of that magnitude anywhere in the global community was everybody’s business. He started to push for an acceleration of pandemic preparedness, including COVID-19 testing, in the United States.
Around the same time, warning bells were similarly ringing for infectious-disease epidemiologist Jennifer Nuzzo. She became increasingly dismayed in the months that followed, watching rates of morbidity and mortality rise around the globe because of a general lack of preparedness for disease outbreaks. In April, she took on a position as director of the newly established Pandemic Center at Brown University School of Public Health in Providence, Rhode Island, so she could work to ensure the world never again finds itself so unprotected. She says governments and other organizations around the world must take action now to make sure that, when the next pandemic inevitably emerges, health-care professionals will be empowered to stop the spread earlier and limit its impacts.
Curbing infectious disease rests on several medical pillars. The ability to identify outbreaks as they emerge in frontline settings, and sharing that information with other institutions, is important. So, too, is the preparedness of health-care providers to respond when pandemics do hit; clear, well-drilled plans of action and secure access to vaccines and other essential medical supplies are crucial. And not just for some nations: the world’s ability to find and stop the next pandemic is only as good as its weakest link.
Frontline vigilance
Disease outbreaks can be caused by various types of pathogen, including viruses, bacteria, fungi and parasites. Finding a pathogen with pandemic potential starts with testing people who are ill, and finding out exactly which pathogen is causing their symptoms.
Cecilia Sorensen, an emergency medicine physician and director of the Global Consortium on Climate and Health Education at Columbia University in New York City, describes hospital emergency departments as “sentinel systems” for infectious disease, because they’re often the first places people go to when experiencing unusual symptoms. “That decision point in emergency rooms sets the stage for what happens next,” she says.
Often it’s the emergency medicine physicians who make decisions about what information to gather from a person through laboratory testing, at least initially. Sorensen emphasizes that, in a pandemic-aware world, these professionals need to be meticulous about diagnosis, staying alert to symptoms that don’t fit the typical pattern for the region. “Emergency providers need to have a really high index of suspicion,” she says. Maintaining frontline health-care professionals’ awareness of what might be spreading in another region, as well as what is endemic in their own, can help to prompt diagnoses that they otherwise might not have considered. But in reality, Sorensen says, the supply of this valuable information to those on the front lines is inconsistent.
The ability of medical personnel to correctly diagnose an infection also depends on hospitals’ disease-testing capacity. Inglesby pushed for testing in the early days of the COVID-19 pandemic, so that medical teams could find out for certain whether they were dealing with the new pathogen that was spreading around the world. The US Centers for Disease Control and Prevention (CDC) created such a test, but Inglesby thinks that it did not find its way into clinical labs and public-health settings quickly enough.
At present, the diagnostics available in any given hospital usually reflect the illnesses they most commonly encounter. As a result, health-care workers often do not have easy access to tests that would allow them to confirm an unusual illness for their region, as might be the case in the early days of a pandemic. To rectify this, Sorensen thinks that hospitals should establish relationships with laboratories that can test for diseases that aren’t in their own wheelhouse, so that these labs can be called on quickly when needed. In the United States, for example, a hospital in Colorado that might not regularly test for tick-borne Lyme disease could develop a relationship with a laboratory in the northeast of the country that does so regularly.
Senjuti Saha, a molecular microbiologist and director of the Child Health Research Foundation in Dhaka, says that the range of available diagnostics in hospitals in low- and middle-income countries is often particularly limited—physicians commonly encounter illnesses for which they cannot identify a cause. Not only does this reduce the likelihood that people will get appropriate treatment, but it also tends to mask outbreaks, since it remains unclear whether illnesses in an area are caused by many different pathogens or the same one.
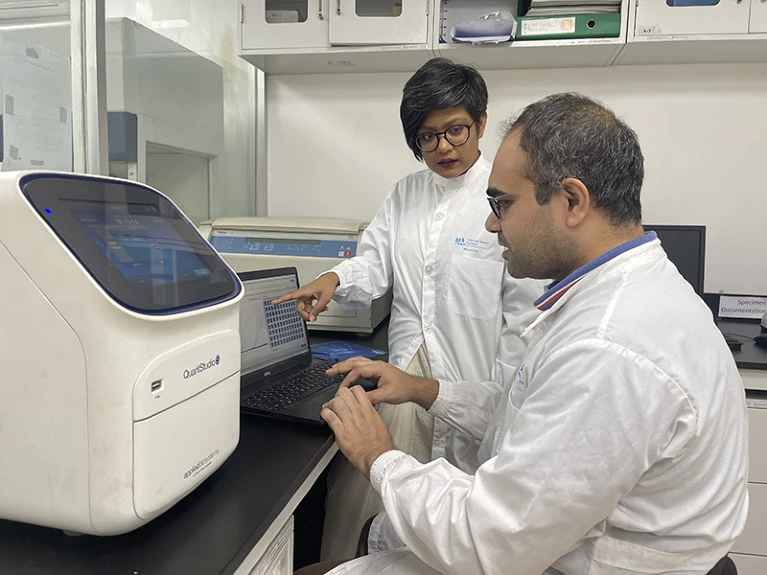
Genomic testing can be a helpful tool in these cases. Saha’s group has used a genomic sequencing facility to analyse cases of meningitis in the local community that were caused by unknown pathogens. Sequencing samples of cerebrospinal fluid from children who had meningitis showed, to the researchers’ surprise, that in some cases their condition stemmed from an otherwise unnoticed outbreak of the chikungunya virus, a mosquito-borne pathogen. This allowed the group to design a test for the pathogen that the nearby hospital’s diagnostic lab could use in future to detect outbreaks of the virus faster.
Others are trying to replicate Saha’s setup. A report from the World Health Organization (WHO) in March laid out how to use genomic data as part of broader surveillance of pathogens with epidemic and pandemic potential1. And the Africa Pathogen Genomics Initiative, backed by several governmental and philanthropic organizations, is supporting efforts to increase the use of genomic sequencing for disease surveillance across the continent.
Sharing and comparing
Obtaining accurate information about disease occurrence in a single hospital or region is the first step in preventing future pandemics. The next is to ensure that data collected by various health-care providers and testing labs are shared and collated, to allow health organizations and government officials to grasp the bigger picture.
Although the International Health Regulations, signed by 196 countries, include a commitment to share information about extraordinary disease outbreaks with the rest of the world, individual countries sometimes struggle to coordinate even their own internal data. Early in the COVID-19 pandemic in the United States, for example, health officials in many states collected information from hospitals but were not required to send the disease data to the federal government. This hampered efforts to create an overall picture of cases in the country. Congress later passed laws requiring hospitals and states to share data with federal officials, but this is COVID-19-specific and not expected to be permanent. Inglesby says better federal authority to get information on infectious-disease outbreaks from US states should be a high priority. “We need to be ready for the next pandemic and not have to wait for new legislation,” he says.
Tieble Traore, technical officer for emergency preparedness at the WHO’s regional office emergency hub in Dakar, says that after the Ebola outbreak in West Africa between 2014 and 2016, the WHO has led efforts to strengthen information-sharing practices in Africa. Under a strategy adopted in 2016, health officials now encourage robust community participation to improve data sharing about threats to public health. Health-care workers and volunteers—ranging from local political and religious leaders to birth attendants—identify potential health problems in the community and report the information by text message to their nearest health facility. If a serious public-health problem is suspected, the health facility is required to report data on disease cases to the district, regional or national level within 24 hours for further scrutiny.
Data sharing and integration is being improved globally, too. The Rockefeller Foundation, a medical research organization based in New York City, is collaborating with a health-research foundation, Wellcome, in the United Kingdom to develop an independent early-warning system to detect emerging pathogens (or new variants of known pathogens) so they can be quickly contained. The system is based on technology that pulls together disparate data sets for analysis. The UK government has also launched a surveillance network called the Global Pandemic Radar in partnership with the WHO and several other organizations, to track disease outbreaks wherever they occur. The initiative expands surveillance infrastructure and data sharing agreements already in place for other infectious diseases, such as HIV, tuberculosis and malaria.
A state of readiness
In the best-case scenario, a local disease outbreak is promptly detected and controlled. But should a cluster of disease somewhere in the world grow into a pandemic threat, health-care systems everywhere must be ready to mount a response.
Nuzzo thinks that practice drills for infectious disease crises are crucial for pandemic prevention. Exercises similar to fire or earthquake drills support a culture of preparedness, and create an understanding among medical providers that outbreaks will continue to happen and that a complete shutdown is not the only option. Hospitals and government health agencies must not only plan for pandemics, Nuzzo says, but also “regularly exercise those plans so that they’re not dusty and unknown when the outbreak happens”.
Taiwan, for example, conducts a vaccination drill every year in the form of a seasonal influenza mass vaccination campaign2. Unlike more haphazard approaches to flu vaccination in some countries that might see shortages, or doses slowly distributed across a season, the exercise simulates a rapid medical countermeasure during a pandemic, in which vaccines or medicines would need to be distributed widely and rapidly. Not only does it familiarize the general public with where to access vaccines in an emergency, but it also creates relationships between the different stakeholders who assist with emergency medical preparedness. Traore says that staff in the WHO African region also emphasize the need for training or simulation exercises to maintain operational readiness.
In addition to being well-drilled, a good response to a pandemic also relies on having the capacity to handle a spreading disease—a particular issue in resource-limited settings. “Capacity comes from access,” says Desiree LaBeaud, a paediatric infectious-disease specialist at Stanford University in California who collaborates with researchers in Kenya. “Access to knowledge, access to diagnostics, treatments, vaccines, medical care, and then trained individuals and social capital.” Without this capacity, local health professionals might quickly become overwhelmed during a disease outbreak, leaving the population vulnerable.
Researchers have called for further investigation of best practices for building capacity in the most challenging global settings, such as places with protracted conflicts or political instability3. Global partnerships and relationships, however, can aid this capacity informally for many low- and middle-income countries, provided the relationships are built long before a pandemic puts them to the test.
One crucial aspect of capacity-building is vaccines. With emerging pathogens, developing and manufacturing a vaccine must happen quickly. Efforts are under way to streamline vaccine development and production: for example, an international foundation called the Coalition for Epidemic Preparedness Innovations is spearheading a campaign for research that will allow vaccines to be developed for new pathogens within 100 days of identification. And researchers have proposed a 10- to 20-year investment in leveraging knowledge of ‘prototype’ viral pathogens from each known family or genus to develop vaccine candidates in case they are needed.
Inglesby says that once a safe, effective vaccine is developed for a pathogen, systems need to be in place to manufacture at scale, all around the world. This would require working with industry, ensuring the right financing and partnerships for technology transfer. “It shouldn’t be the case that one or two countries have most access to a vaccine because the vaccine is produced in those countries,” he says. LaBeaud concurs, and points out that if COVID-19 vaccines had been distributed more equitably, we might not have had to deal with variants that subsequently arose.
Some efforts have been made to establish international, multi-disciplinary health teams that can snap into action anywhere in the world when an outbreak reaches a certain scale. The WHO-led Global Outbreak Alert and Response Network is made up of more than 150 organizations committed to tackling pandemics in their early stages4, although it relies heavily on volunteers. Bill Gates has proposed a similar network, which would use a group of fully paid international pandemic responders. But Saha advocates building local, decentralized capacity, in Bangladesh and other countries, to decrease reliance on help from others that might vanish in times of crisis.
For her, capacity building is about reducing ‘parachute science’, in which researchers from resource-rich countries enter resource-limited places and “get their shoes dirty for an afternoon”. “The samples flow out of the country, analysis is done somewhere else, and we lose our ownership,” she says.
Instead, Saha would rather see local scientists learn how to use the necessary technologies and get excited about solving problems with them. “A lot of the work we do as scientists comes from passion,” Saha says. “If you don’t have that passion, if you haven’t handled the sequencing yourself, there’s no way you’ll be able to explain it to a policymaker or advocate for change.”
Nuzzo is optimistic that COVID-19 can create an awareness of, and commitment to, pandemic preparedness. She compares the situation to the devastating fires in US cities at the turn of the twentieth century that sparked a shift in fire safety and preparedness in the country. Fire departments help to prevent uncontrolled blazes ruining lives; sustained funding of pandemic preparedness could do the same thing for infectious-disease outbreaks. In June, the World Bank approved the creation of a global fund to strengthen pandemic prevention, preparedness and response activities, intended to help close gaps in capacity.
Inglesby stresses that, to stay on top of infectious diseases, health-care providers at every level must take responsibility, whether they are international organizations, government agencies, states or regions, or local hospitals. “Sustained leadership commitment and awareness is what will make everything possible,” he says. And as the COVID-19 pandemic has made abundantly clear, the whole world must be prepared. “We’re all together on this one little planet, working together,” says LaBeaud. No pandemic response, however well thought out and funded, can be truly effective if it is applied in just one portion of the globe.
This article is part of Nature Outlook: Pandemic Preparedness, an editorially independent supplement produced with the financial support of third parties. About this content.
References
-
World Health Organization. Global Genomic Surveillance Strategy for Pathogens with Pandemic and Epidemic Potential, 2022–2032 (WHO, 2022).
-
Meyer, D. et al. Am. J. Public Health 108, S188–S193 (2018).
-
Saleh, S., Mansour, R., Daou, T., Brome, D. & Naal, H. Confl. Health 16, 31 (2022).
-
Mackenzie, J. S. et al. Glob. Public Health 9, 1023–1039 (2014).

