The emergency phase of COVID-19 might have passed, but it remains fresh in the minds of politicians and the public.
This is a unique moment to learn from the global response. More outbreaks of infectious disease are inevitable. But it is possible to stop many of them turning into pandemics. The past 20 years of outbreaks—not only of COVID-19, but also Zika, Ebola, swine flu, Middle Eastern respiratory syndrome (MERS) and severe acute respiratory syndrome (SARS)—can teach us how to improve global health security. Preparing for future pandemics involves strengthening the entire chain of the outbreak response, from identifying a pathogen through to mass vaccination.
Monitor zoonoses
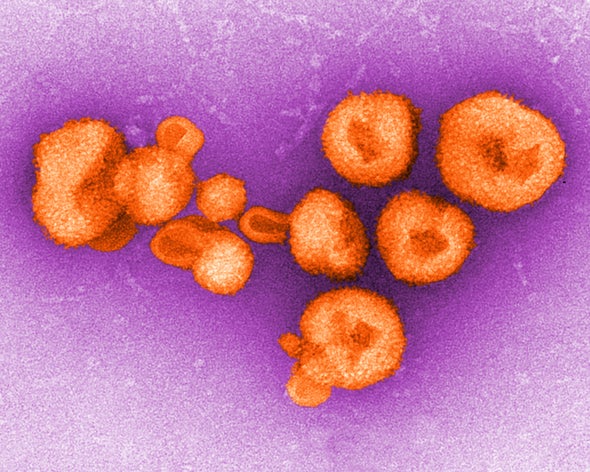
The biggest risk comes from pathogens that circulate in animals making the jump into humans. As COVID-19 has demonstrated, once someone is infected in one part of the world, trade and travel will rapidly carry the virus nearly everywhere else. Assessing which pathogens are most likely to make the jump enables us to prepare vaccines and treatments. The World Health Organization has identified several priority diseases with pandemic potential, including Crimean–Congo haemorrhagic fever, Ebola, Marburg, Lassa fever, MERS, SARS, Nipah virus infection and Zika.
However, there are many pathogens with pandemic potential circulating in animals that we do not know about. It is crucial to identify hotspots where humans and animals come into contact and take steps to reduce risk. For example, hygiene standards at markets where animals are slaughtered and sold could be more closely regulated.
Sequence globally
To develop the tools required to tackle a pandemic, such as diagnostic tests, vaccines and therapeutics, we must know what we are fighting. It is crucial that we quickly obtain and share the genetic sequences of viruses as they emerge.
This was done remarkably well with SARS-CoV-2—not only for the original sequencing in China, but also for subsequent variants detected elsewhere. But not all countries have this capability. If a virus emerges in a country without the ability to sequence it then it could spread silently for weeks, as happened when Ebola surged in Guinea in 2014. To avoid delaying responses that could be crucial to stopping a pandemic, such as reformulating vaccines, there must be investment in genetic-sequencing capability everywhere.
Strengthen manufacturing
Swine flu, COVID-19 and monkeypox have shown that the model of charitable donations of vaccines from wealthier countries does not work. This leads to vaccine inequality: high-income countries control access to the bulk of supply, and low-income countries get very little. COVID-19 revealed the fragility of vaccine production. The world is heavily dependent on just a few manufacturers, such as the Serum Institute of India in Pune. The manufacture of vaccines and therapeutics needs to be spread more equitably, with regional hubs ready to mass produce high-quality medical products in an emergency. Building local manufacturing capacity requires waiving intellectual-property rights, building factories and training people to work in them—often in low-resource settings. This necessitates the participation of the private sector alongside governments, given its role in vaccine research, production and distribution.
Prepare vaccines for rapid production
Vaccination is essential to beating viral pandemics. If vaccines are ready in advance, they can be quickly deployed when threats emerge to help contain the spread. For pathogens with known pandemic potential, such as influenza, governments should invest in vaccines that can protect against a wide variety of variants. Clinical trials of universal flu vaccines, which mix flu strains to promote a broad-based immune response, are under way. To protect against threats that we have no knowledge of before an outbreak, scientists are creating plug-and-play technical platforms, such as mRNA technology or adenovirus vectors, that can be quickly modified to combat a specific emerging threat.
Stop the spread
Finally, governments must abandon the idea that spread of a respiratory pathogen is inevitable. During the COVID-19 pandemic, countries such as Sweden and the United Kingdom dismissed the idea of a vaccine being ready quickly enough to protect the bulk of the population from infection. Yet multiple vaccines were created, trialled and approved in roughly a year. How many people would have lived if governments had worked to stop transmission until mass vaccination campaigns rolled out? All reasonable efforts should be made to delay the spread of a virus until medical interventions are available. This includes enacting emergency mask mandates in public settings, such as shops and transport hubs, and making plans to keep schools open by moving classes to stadiums, museums and other large spaces that can provide a safer environment.
These five steps can help us respond to pandemic threats better than before. Some progress has been made: the 100 Days Mission, presented to leaders of the G7 group of the world’s biggest economies in 2021, includes each of these points in its roadmap for moving from sequencing to vaccines within 100 days. It is of utmost importance that gains are maintained and more investments in pandemic preparation are made, even as the memory of the COVID-19 crisis fades from politicians’ minds. We have identified solutions for the future—now we must act on them.
This article is part of Nature Outlook: Pandemic Preparedness, an editorially independent supplement produced with the financial support of third parties. About this content.