During an embryo's development, a piece of the still-growing brain branches off to form the retina, a sliver of tissue in the back of the eye. This makes the retina, which is composed of several layers of neurons, a piece of the central nervous system. As evidence builds that changes in the brain can manifest in this region, scientists are turning to retinas as a potential screening target for early signs of Alzheimer's, an incurable neurodegenerative disease that affects an estimated six million people in the U.S. alone.
Initially clinicians could diagnose Alzheimer's only through brain autopsies after patients died. Since the early 2000s, however, research advances have made it possible to pinpoint signs of the disease—and to begin to investigate treatment—years before symptoms first appear. Today positron emission tomography (PET) brain imaging and tests of cerebrospinal fluid (CSF), the clear liquid surrounding the brain and spinal cord, aid Alzheimer's diagnosis at its early stages.
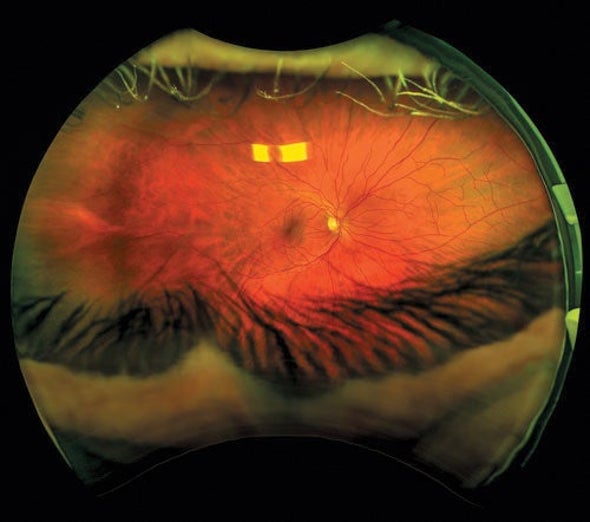
“There have been tremendous improvements in our ability to detect early disease,” says Peter J. Snyder, a neuropsychologist and neuroscientist at the University of Rhode Island. But these diagnostic methods are not always readily available, and they can be expensive and invasive. PET imaging requires injecting a radioactive tracer molecule into the bloodstream, and spinal fluid must be extracted with a needle inserted between vertebrae in the back. “We need ways of funneling the right high-risk individuals into the diagnostic process with low-cost screening tools that are noninvasive and simple to administer,” Snyder says. The retina is a particularly attractive target, he adds, because it is closely related to brain tissue and can be examined noninvasively through the pupil, including with methods routinely used to check for eye diseases.
One approach to retinal screening aims to search for signs of beta-amyloid, the peptide that amasses into damaging plaques in the brains of people with Alzheimer's. Studies suggest this protein fragment also accumulates in the retina—and researchers have found evidence that it may be detectable there before the onset of symptoms.
In 2014 Robert Vince and Swati More of the University of Minnesota's Center for Drug Design first described how to use a method called hyperspectral imaging, which captures an image at many different light wavelengths, to identify amyloid aggregates (clumps of beta-amyloid) in mouse retinas. They then confirmed these clumps in the animals' brains at later stages of disease. Since first reporting those findings, the two scientists and their colleagues found that amyloid aggregates may act as an early marker in human eyes, too.
The team has since licensed the technique to a Canadian medical imaging company, RetiSpec, which combines it with a machine-learning algorithm that pinpoints amyloid clumps in hyperspectral images. Investigators at multiple facilities across North America are now conducting clinical trials to examine this technique's efficacy.
Preliminary findings from the trials, presented at a conference last November, included 108 participants who either were at risk of or had preclinical Alzheimer's or mild cognitive impairment, which can be an early sign of neurodegenerative disease. After comparing the retinal screening tests with PET and CSF results, the researchers found the technique correctly identified people with brain amyloid 86 percent of the time and correctly ruled out those without it 80 percent of the time. These results are promising, says Sharon Cohen, medical director at Toronto Memory Program and leader of the trial. More data are needed before this can be rolled out as an approved diagnostic tool, Cohen adds. “But I think that day will come.”
Other researchers have also reported amyloid in the retinas of people whose PET scans show amyloid plaques but who do not show signs of cognitive decline. University of California, San Diego, neuroscientist Robert Rissman and his colleagues are conducting retinal screens in participants taking part in a larger, ongoing trial of an investigative Alzheimer's drug for this population. The investigators measured retinal amyloid in a small feasibility study of eight participants, and they are now screening retinas among a larger number of patients—both before and after treatment. These data may illuminate how retinal amyloid changes over time and show whether their treatment reduces its levels, Rissman says.
Scientists are also focusing on other retinal signs of early Alzheimer's. In a study published earlier this year in JAMA Ophthalmology, researchers reported that retinal thickness was associated with certain aspects of cognitive performance. And Snyder's team has been investigating progressive changes in the retina's anatomy, such as shrinkage in certain regions; preliminary work seems to indicate a correlation with amyloid buildup in the brain. Snyder and his colleagues are now looking for these and other retina-based biomarkers, such as changes in blood vessels, as part of a longitudinal trial known as the Atlas of Retinal Imaging in Alzheimer's Study (ARIAS).
Although there are a variety of approaches to retina-based diagnosis, Rissman says that they remain unproved at this stage. He cautions that there are several open questions—including whether the protein aggregates that researchers detect are actually amyloid. Snyder points out that scientists are still debating the best method of identifying the substance in retinas and that findings from imaging studies of these protein clumps have sometimes varied from one facility to another.
Cohen, however, says that “while additional confirmatory studies in different laboratories … are always welcome, there is sufficient evidence of amyloid deposition in the retina such that the finding should no longer be in dispute.”
Early detection and accurate diagnosis are key to getting people on the right care and treatment path—and tools such as retinal imaging can aid both patients and physicians in that journey, says Rebecca Edelmayer, senior director of scientific engagement at the Alzheimer's Association. Even though the full potential of retinal imaging has yet to be determined, she adds, “it's a really interesting time in this space.”